SLE myelitis is the only example that calls for immunosuppression. In gray matter myelitis—characterized by an irreversible flaccid paraplegia that comes on very quickly—corticosteroids can be given in the prodromal period, otherwise they won’t work, Dr. Birnbaum said. In white matter myelitis—which comes with milder weakness and is relapsing—immunosuppressive therapy is called for, he said.
Demyelinating Syndrome in Sjögren’s Syndrome
Again, Dr. Birnbaum advised clinicians to be skeptical, even when an MRI suggests a demyelinating syndrome in SS. There must be clinical evidence, such as optic neuritis, myelitis or brainstem syndrome, he said.
“It’s not enough to have vague neurological complaints,” Dr. Birnbaum said. “If your Sjögren’s patient does not have a demyelinating syndrome, no matter what the MRI is showing, it’s very unlikely the patient has an underlying demyelinating disease.”
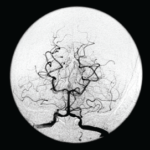
Two potential candidates for an underlying demyelinating disease are neuromyelitis optica (NMO) and multiple sclerosis (MS).
In MS, spinal cord inflammation comes in a transverse pattern; however, it’s longitudinal in NMO; the clinical features of MS are initially sensory with mild motor weakness, and in NMO there is greater weakness; there are no autoantibody markers for MS, but NMO is marked by the NMO-IgG antibody. And MS treatment typically involves immunomodulatory medication, and NMO calls for immunosuppressants.2
In recent years, about half of Sjögren’s patients were defined as having NMO, but there have been only sparse reports of MS in Sjögren’s, he said. Most of the literature on MS as a Sjögren’s complication was published before NMO was recognized as its own entity.
He noted that the aquaporin 4 protein—antibodies to which (NMO-IgG) are a marker of NMO—is enriched in the end organs targeted in Sjögren’s.
“It really, really suggests that neuromyelitis optica, and not multiple sclerosis, is the salient demyelinating syndrome seen in Sjögren’s,” he said. “And further study is warranted to see whether this is a causative relationship.”
Thomas R. Collins is a medical writer based in Florida.
References
- Hanly JG, McCurdy G, Fougere L, et al. Neuropsychiatric events in systemic lupus erythematosus: attribution and clinical significance. J Rheumatol. 2004 Nov;31(11):2156–2162.
- Wingerchuk DM, Lennon VA, Pitock SJ, et al. Revised diagnostic criteria for neuromyelitis optica. Neurology. 2006 May 23;66(10):1485–1489.
Second Chance
If you missed this session at the 2015 ACR/ARHP Annual Meeting, it’s not too late. Catch it on SessionSelect.