In addition, having collected considerable data from our lupus and control cohorts, we were poised to ask a new question: What is the prevalence of atherosclerotic cardiovascular disease in RA compared with that in SLE? Although markers of disease severity in RA have been linked to an increase in overall mortality, the specific aspects of RA or its treatment that might heighten the risk of cardiovascular disease were not known.12,13
Even in the absence of traditional risk factors for atherosclerosis, women with RA had high rates of non-fatal myocardial infarction.14,15 Corticosteroids did not appear to increase the risk of cardiovascular events, while therapy with methotrexate was associated with lower all-cause mortality, largely due to a reduction in cardiovascular mortality, suggesting that some treatments of RA might mitigate cardiovascular risk.16 As was the case for SLE, however, most published work was retrospective, event rates were low, and there were no controls for the impact of conventional risk factors, treatment, and disease activity and severity.
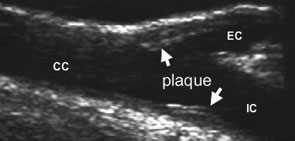
Here again, we assessed the prevalence of atherosclerosis employing ultrasound-defined carotid artery plaque as a direct measure of and proxy for generalized atherosclerosis and as a surrogate for coronary atherosclerosis. We recruited 98 RA patients who were matched with controls and SLE patients on the basis of age (± five years), gender, and race.
More Atherosclerosis in Patients with RA
Despite a more adverse risk profile in control subjects (slightly higher blood pressure, more smokers, and lower HDL cholesterol), carotid atherosclerosis was three times more prevalent in the patient group (44% versus 15%, p<0.001).17 The presence of atherosclerosis was higher in RA patients in all decades of life; the difference was particularly striking among younger subjects. In fact, the prevalence of plaque in RA patients was comparable to that in SLE, a most dramatic and unexpected result. (See Figure 2, below.) The association between RA and atherosclerosis remained after accounting for age, cholesterol, smoking history, and blood pressure.17
Although others have found increased intimal-medial thickness in RA, intimal-medial thickness did not differ between RA patients and controls. This result is comparable to our findings in SLE patients, indicating that intimal-medial thickness does not invariably correlate with atherosclerosis, particularly in relatively young individuals with chronic inflammatory disease. Indeed, plaque is the unequivocal manifestation of atherosclerosis, and a more potent predictor of adverse cardiovascular outcomes than intimal-medial thickness.

