Pathophysiology Unpacked
In 1951, Dr. Schick personally translated Die Serumkrankheit into English. In his preface, he noted that interest in the monograph had grown over the years and stated, “All our allergy tests and almost everything we know about allergic diseases have their origin in the observations in serum sickness which contain passive transfer and serum sickness in ‘reverse.’”
In the 1950s, work done by Fred G. Germuth Jr., MD, Frank J. Dixon, MD, and other investigators began to further elucidate the pathophysiology of serum sickness.5,11,12 Dr. Atkinson explains that much of this work was done in rabbit models. “You would keep injecting and look in the kidney. You could look at tissues though microscopes; you could stain things that you couldn’t in the ’30s or ’20s. [Researchers] intensively studied these models to find out what was causing the damage in the kidneys and the joint swelling.”
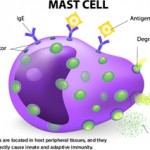
The findings clearly demonstrated that circulating immune complexes were responsible for serum sickness. The researchers observed that foreign proteins injected into animals caused a strong antibody response and that this antibody combined with the injected antigen to form circulating complexes. These immune complexes could then activate complement and cause tissue damage, such as arteritis and glomerulonephritis.8
But these findings had implications beyond understanding serum sickness itself. “When I first got into the field as a house officer in the last ’60s and early ’70s, what first got me interested in serum sickness was the fact that lupus patients had similar manifestations,” Dr. Atkinson explains. He notes that 50 years after serum sickness was first described, papers were showing some of the pathogenesis of lupus seemed to be serum sickness-like. He adds, “In the sickest lupus group, C3 and C4 are still used in almost every categorization I know of, as are autoantibodies, as is kidney disease and skin manifestations and joints—all those things you get in lupus that you can also get in serum sickness.”
Modern Parallels
Investigators are still exploring how antibodies sometimes result from modern treatments, causing side effects and reducing efficacy. This is true for some compounds chemically modified with polyethylene glycol (PEG). For example, pegloticase (Krystexxa) is a recombinant PEGylated uricase approved for adults with refractory, chronic gout. Although the treatment appears to be highly effective in a subset of individuals, many quit responding over time.13 This loss of responsiveness is associated with the development of higher titers of anti-pegloticase antibodies. These increase the clearance of pegloticase, and they are also associated with an increased risk of infusion reactions.14
“Unfortunately, the immune response to pegloticase is limiting its utility, but there are lessons to be learned from the experience with another PEGylated treatment, pegvalaise,” says Dr. Atkinson.
Dr. Atkinson draws a parallel between Pirquet and Schick’s characterization of serum sickness and a recent, exceptionally detailed description of a chronic serum sickness-like illness, this time in response to PEGylated enzymes used to treat phenylketonuria (PKU). The devastating neurological disease results from a genetic deficiency in an enzyme that metabolizes phenylalanine, leading to elevated blood levels.
Pegvaliase, developed by BioMarin, is a bacteria-derived recombinant phenylalanine ammonia lyase (PAL), an enzyme that catalyzes the conversion of phenylalanine into other products. In pegvaliase, investigators conjugated PAL with polyethylene glycol.15
Dr. Atkinson notes, “Now, many drugs are being PEGylated. One reason is to give them a longer half-life. Another is to try and cover them up so they aren’t so immunogenic. In pegvaliase, it probably does some of both.” He also explains that because PEGylated compounds are found so commonly in our environment (in foods, perfumes, other products), many people are already carrying antibodies to them.
Enzyme replacement therapies, such as pegvaliase, often induce anti-drug antibodies that can cause hypersensitivity reactions (potentially mediated via immune complex formation). Such antibodies can also reduce efficacy through the formation of neutralizing antibodies. Moreover, anti-PEG antibodies have been documented in several reports. The investigators at BioMarin wanted to characterize this more deeply in the specific case of pegvaliase to help develop a dosing protocol that optimized safety and efficacy.15
Dr. Atkinson is one of the collaborators on the 2018 study that explored the immunogenicity of pegvaliase, characterizing its safety and efficacy. “We did this very detailed look in a setting where we could control many factors,” he says. “Compared even to 20 years ago, some of those things couldn’t have been done. You know how much antigen you are giving; you are measuring the IgG responses and the IgM; you have the ability to monitor what happens to the antigen, the drug.”
The BioMarin group extensively monitored patients taking pegvaliase, recording clinical data, measurements of antibody titers of multiple isotypes and specificities, assessments of enzymatic neutralization, immune complexes and biomarkers for complement activation.15
In the first six months after treatment initiation, IgG and IgM anti-PEG antibodies were present, as well as IgG and IgM anti-PAL antibodies. Later in treatment, anti-PEG antibodies decreased to baseline levels. Circulating immune complexes were found to be highest in early treatment, and they decreased over time. Hypersensitivity symptoms were also most frequent early on, decreasing as immune complex formation lessened and as complement levels rose. This allowed the dosage of pegvaliase to be titrated gradually upward, so the drug could reach efficacious levels while minimizing risks. With the increased dose of pegvaliase and maturation of the immune response, blood phenylalanine levels decreased over time.15
Some patients receiving therapeutic anti-sera in the early 20th century received repeated doses when they were thought to be re-exposed. However, administration of the foreign serum was not chronic, in contrast to ongoing treatment with pegvaliase. This ongoing administration creates its own hazards and challenges, as it does for pegloticase.
As Dr. Atkinson explains, “They were able to treat these patients for several years. Despite having low C3, low C4, and despite antibodies developing, they got away with it.
“The antibodies kind of leveled off. Despite giving more antigen, the majority of the patients sort of plateaued. Because they didn’t get any IgE antibodies, it’s not an acute allergic reaction, which would be another thing to consider.” He concludes, “So I think it is a form of chronic serum sickness.”