In 1905, two pediatricians in Vienna, Austria, published Serum Sickness, a detailed 120-page monograph that was the first to carefully characterize the syndrome.1 The work would go on to become a classic, ultimately helping illuminate many important questions in immunology.
Antitoxin Serum Treatments
In the late 19th century, researchers were working to develop lifesaving antitoxins to certain bacterial diseases.2 Scientists learned how to harvest toxins from bacteria grown in a laboratory. They would then inject horses or other animals with the toxin, and the animals’ immune systems would produce an antitoxin. This could then be collected from the animals, purified and administered as a serum. The antitoxin could successfully neutralize the effects of the original bacterial toxin, such as Corynebacterium diphtheriae.3
Tetanus antitoxin was discovered in 1890, and the first case of diphtheria treated with antitoxin was described the following year.2 Such antitoxins soon became common in clinical practice. Clinicians could treat infected persons with them or use them prophylactically in some situations, such as to control disease outbreaks. Anti-serum injections of C. diphtheriae gave patients immunity for around three weeks.4
Dr. Atkinson
According to John P. Atkinson, MD, the Samuel B. Grant Professor of Medicine at Washington University, St. Louis, School of Medicine, “It was pre-antibiotics. Initially this was the only treatment that had been shown to be effective.”
Quickly, it was recognized that though they could save lives, antitoxin serums sometimes caused side effects. Rarely, rapid anaphylactic-type responses were observed after a person was injected with serum.
But another type of response was almost universally observed, initially termed serum exanthema. These self-limited responses were not life threatening and were deemed relatively insignificant. However, the process of coming to understand these responses would contribute to a wider understanding of many important processes in immunology.1,5
Die Serumkrankheit (Serum Sickness)
From 1903 to 1910, Viennese pediatrician Clemens Freiherr von Pirquet, PhB, MD, made very detailed and important observations that helped provide foundational work for the fields of immunology and allergy.5 The studies put forth in Die Serumkrankheit were key components. He wrote the monograph in collaboration with Béla Schick, MD, a Hungarian-born pediatrician with whom he worked at the University of Vienna as lab assistant to Theodore Escherich (known for his work on Escherichia coli).6

Dr. Pirquet
Arthur M. Silverstein, PhD, an immunologist, science historian and professor emeritus of ophthalmic immunology at Johns Hopkins School of Medicine, Baltimore, says, “It really was a phenomenal, remarkable piece of work.”
“It is beautifully done,” Dr. Atkinson adds. “It’s very logical and thought provoking and has great attention to detail. You read paragraph after paragraph about issues that came up: How much serum was administered and where, which disease was being treated, patients’ ages, how sick they were, the timing of everything. All these things were carefully documented in what we might call a long clinical article.”
The pair became the first to describe the syndrome in detail and the first to propose that serum sickness arose as a product of an immunological process.5
Clinical Description
The first part of the monograph, “Clinical Aspects of Serum Sickness,” makes up more than half of the text. Here, Pirquet and Schick explored the nature of symptomatology and disease course, referencing case studies of adults and children gathered in their clinic work. They provided detailed graphs showing the timing of specific clinical symptoms as well as laboratory findings, such as leukocyte numbers and blood precipitins.
At the outset, they renamed the syndrome. They wrote:
We have abandoned the expression ‘serum exanthema’ because we think that this name could easily lead to the idea that the rash was the most important symptom of the disease; in its place we have proposed the name ‘serum disease’ or ‘serum sickness.’
Pirquet and Schick were careful to document timing in patients who had never been exposed to anti-sera before:
Most frequently the symptoms of disease start suddenly between 8 and 12 days after the injection … . The period of incubation cannot be explained by the slowness of the absorption of the foreign serum. This serum exerts its anti-toxic effect within a few hours.
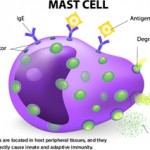
Dr. Atkinson confirms this timing coincides with what we now know about antibody production. “It takes humans five or six days to make antibodies. The IgM comes up, and a few days later the IgG comes up. Then it interacts with the horse serum—immunoglobulin and other proteins, depending on how clean and pure it was. Depending on the ratios and the precipitation reaction, it can form immune deposits in the kidneys and in the joints. Then, as you clear it out within a couple of days, it all goes away.
“The rash and fever were two of the most common problems,” adds Dr. Atkinson. “They described the fevers, how high they were and how long they lasted. Quite a few patients got joint pains, and they go through which joints, whether symmetrical or non-symmetrical. They mention that a few patients had albuminuria.” The pair also noted such symptoms as enlarged lymph nodes and edema, which they documented carefully through tracking patients’ weights.
Pirquet and Schick also made key insights into the relationship of serum dosage to symptom onset, noting:
The intensity of the symptoms also becomes decidedly stronger with an increase in the amount of serum … . The prophylaxis of serum sickness consists in the first place in using the smallest possible amount of serum.
Readministration
In the second section of the monograph, Pirquet and Schick carefully documented the differences in patients receiving a second dose of serum. They observed a large group of children who received diphtheria anti-sera due to exposure on a clinical ward. They then noted the differences between children who had previously received injections and those who had not. Those who had been reinjected often showed an accelerated response, sometimes within 24 hours. They wrote:
This difference could not be due to the antigen (injected serum), as we have shown in our experiments, since the same serum caused different kinds of differently timed reactions, depending on whether it was injected into the organism for the first time or was reinjected. Thus we came to the conclusion that it was the human organism which has become specifically altered, due to the injection of a foreign serum.
‘What first got me interested in serum sickness was the fact that lupus patients had similar manifestations,’ explains Dr. Atkinson. … ‘In the sickest lupus group, C3 & C4 are still used in almost every categorization I know of … .’
Theory of Serum Sickness
In the final section, Pirquet and Schick pulled together research from the existing human and animal literature and speculated about disease pathophysiology. Confusing the issue, the clinical manifestations did not completely coincide with the presence of precipitins found in the serum, which made the role of antibodies unclear.7 However, they posited that the symptoms of serum sickness were created by a chemical reaction between the horse serum and the patient’s antibodies.
They proposed:
We state the theory that there exists a causal connection between the formation of antibodies and [serum sickness].
As if to anticipate the resistance they were likely to receive, the two wrote:
The conception that the antibodies, which should protect against disease, are also responsible for the disease, sounds at first absurd. This has as its basis the fact that we are accustomed to see in disease only the harm done to the organisms and to see in the antibodies solely antitoxic substances.
They closed the monograph with a testament to their belief in the study’s worth and potential impact:
We believe to have shown that [serum sickness] has great importance, not only from a clinical viewpoint but also from the standpoint of general pathology: serum sickness is the best paradigma [sic] for a disease due to an organic cause which is unable to multiply, and is an exquisite object for the study of the changes going on in the system.
Follow-up & Response
Dr. Pirquet expanded on many of the ideas present in Die Serumkrankheit in his 1910 book, Allergy, written when he was a professor of pediatrics at Johns Hopkins. Here, Dr. Pirquet coined the term allergy (from the Greek roots “strange activity”).5 Since then, the term has taken on a more specific meaning, but then the distinction between allergy and immunity was not as clear.7
Dr. Silverstein explains, “In Allergy he tried to put together the observations that were known at the time, like skin reactions, the tuberculin reaction, serum sickness and anaphylaxis.” However, Dr. Silverstein notes that Dr. Pirquet did not think of himself as what we would call an allergist. He says, “There were no allergists at the time. People didn’t yet understand allergy and its basis.”
In Allergy, Dr. Pirquet made further observations, analyses and speculations about the pathogenesis of serum sickness. Here, he correctly identified immune complexes consisting of antigen and antibodies (“toxic bodies”) as the precipitating factor of the syndrome.5
Dr. Silverstein relates that for the most part, the importance of Die Serumkrankheit was not largely appreciated in the medical community. “It just wasn’t understood at the time, or it wasn’t paid attention to, because people were thinking of other things. So it didn’t really stimulate as one might have expected.”
Still, anti-sera treatments continued to be widely used over the next few decades. Although the pathophysiology of serum sickness was not yet proven, investigators during this time confirmed the clinical findings of Pirquet and Schick in several large retrospective studies of patients given such treatments.8,9 With the advent of antibiotics, far fewer people were given heterologous anti-sera. However, anti-sera treatments continued to be used in some applications, such as for the treatment of tetanus, rabies and botulism, and for snake and spider bites.10
Pathophysiology Unpacked
In 1951, Dr. Schick personally translated Die Serumkrankheit into English. In his preface, he noted that interest in the monograph had grown over the years and stated, “All our allergy tests and almost everything we know about allergic diseases have their origin in the observations in serum sickness which contain passive transfer and serum sickness in ‘reverse.’”
In the 1950s, work done by Fred G. Germuth Jr., MD, Frank J. Dixon, MD, and other investigators began to further elucidate the pathophysiology of serum sickness.5,11,12 Dr. Atkinson explains that much of this work was done in rabbit models. “You would keep injecting and look in the kidney. You could look at tissues though microscopes; you could stain things that you couldn’t in the ’30s or ’20s. [Researchers] intensively studied these models to find out what was causing the damage in the kidneys and the joint swelling.”
The findings clearly demonstrated that circulating immune complexes were responsible for serum sickness. The researchers observed that foreign proteins injected into animals caused a strong antibody response and that this antibody combined with the injected antigen to form circulating complexes. These immune complexes could then activate complement and cause tissue damage, such as arteritis and glomerulonephritis.8
But these findings had implications beyond understanding serum sickness itself. “When I first got into the field as a house officer in the last ’60s and early ’70s, what first got me interested in serum sickness was the fact that lupus patients had similar manifestations,” Dr. Atkinson explains. He notes that 50 years after serum sickness was first described, papers were showing some of the pathogenesis of lupus seemed to be serum sickness-like. He adds, “In the sickest lupus group, C3 and C4 are still used in almost every categorization I know of, as are autoantibodies, as is kidney disease and skin manifestations and joints—all those things you get in lupus that you can also get in serum sickness.”
Modern Parallels
Investigators are still exploring how antibodies sometimes result from modern treatments, causing side effects and reducing efficacy. This is true for some compounds chemically modified with polyethylene glycol (PEG). For example, pegloticase (Krystexxa) is a recombinant PEGylated uricase approved for adults with refractory, chronic gout. Although the treatment appears to be highly effective in a subset of individuals, many quit responding over time.13 This loss of responsiveness is associated with the development of higher titers of anti-pegloticase antibodies. These increase the clearance of pegloticase, and they are also associated with an increased risk of infusion reactions.14
“Unfortunately, the immune response to pegloticase is limiting its utility, but there are lessons to be learned from the experience with another PEGylated treatment, pegvalaise,” says Dr. Atkinson.
Dr. Atkinson draws a parallel between Pirquet and Schick’s characterization of serum sickness and a recent, exceptionally detailed description of a chronic serum sickness-like illness, this time in response to PEGylated enzymes used to treat phenylketonuria (PKU). The devastating neurological disease results from a genetic deficiency in an enzyme that metabolizes phenylalanine, leading to elevated blood levels.
Pegvaliase, developed by BioMarin, is a bacteria-derived recombinant phenylalanine ammonia lyase (PAL), an enzyme that catalyzes the conversion of phenylalanine into other products. In pegvaliase, investigators conjugated PAL with polyethylene glycol.15
Dr. Atkinson notes, “Now, many drugs are being PEGylated. One reason is to give them a longer half-life. Another is to try and cover them up so they aren’t so immunogenic. In pegvaliase, it probably does some of both.” He also explains that because PEGylated compounds are found so commonly in our environment (in foods, perfumes, other products), many people are already carrying antibodies to them.
Enzyme replacement therapies, such as pegvaliase, often induce anti-drug antibodies that can cause hypersensitivity reactions (potentially mediated via immune complex formation). Such antibodies can also reduce efficacy through the formation of neutralizing antibodies. Moreover, anti-PEG antibodies have been documented in several reports. The investigators at BioMarin wanted to characterize this more deeply in the specific case of pegvaliase to help develop a dosing protocol that optimized safety and efficacy.15
Dr. Atkinson is one of the collaborators on the 2018 study that explored the immunogenicity of pegvaliase, characterizing its safety and efficacy. “We did this very detailed look in a setting where we could control many factors,” he says. “Compared even to 20 years ago, some of those things couldn’t have been done. You know how much antigen you are giving; you are measuring the IgG responses and the IgM; you have the ability to monitor what happens to the antigen, the drug.”
The BioMarin group extensively monitored patients taking pegvaliase, recording clinical data, measurements of antibody titers of multiple isotypes and specificities, assessments of enzymatic neutralization, immune complexes and biomarkers for complement activation.15
In the first six months after treatment initiation, IgG and IgM anti-PEG antibodies were present, as well as IgG and IgM anti-PAL antibodies. Later in treatment, anti-PEG antibodies decreased to baseline levels. Circulating immune complexes were found to be highest in early treatment, and they decreased over time. Hypersensitivity symptoms were also most frequent early on, decreasing as immune complex formation lessened and as complement levels rose. This allowed the dosage of pegvaliase to be titrated gradually upward, so the drug could reach efficacious levels while minimizing risks. With the increased dose of pegvaliase and maturation of the immune response, blood phenylalanine levels decreased over time.15
Some patients receiving therapeutic anti-sera in the early 20th century received repeated doses when they were thought to be re-exposed. However, administration of the foreign serum was not chronic, in contrast to ongoing treatment with pegvaliase. This ongoing administration creates its own hazards and challenges, as it does for pegloticase.
As Dr. Atkinson explains, “They were able to treat these patients for several years. Despite having low C3, low C4, and despite antibodies developing, they got away with it.
“The antibodies kind of leveled off. Despite giving more antigen, the majority of the patients sort of plateaued. Because they didn’t get any IgE antibodies, it’s not an acute allergic reaction, which would be another thing to consider.” He concludes, “So I think it is a form of chronic serum sickness.”
Ruth Jessen Hickman, MD, is a graduate of the Indiana University School of Medicine. She is a freelance medical and science writer living in Bloomington, Ind.
References
- von Pirquet C, Schick B. Die Serumkrankheit. Leipzig: Franz Deuticke; 1905. English version, translation by Schick B. Serum Sickness. Baltimore: Williams &Wilkins, 1951.
- Becker EL. Elements of the history of our present concepts of anaphylaxis, hay fever and asthma. Clin Exp Allergy. 1999 Jul;29: 875–895.
- From DNA to beer: How did they make diphtheria antitoxin? National Institutes of Health. 2019 Aug (updated).
- Wendt D, Warnere M. Béla Schick and serum sickness. National Institutes of Health. Circulating Now. 2014 Feb 25.
- Silverstein AM. A History of Immunology. 2nd ed. London, England: Elsevier; 2009.
- Wolf IJ. Bela Schick. JAMA. 1968 Jan 1;203(1):44.
- Turk JL. Von Pirquet, allergy, and infectious diseases: A review. J R Soc Med. 1987 Jan;80(1):31–33.
- Lawley TJ, Bielory L, Gascon P, et al. A study of human serum sickness. J Invest Dermatol. 1985 Jul;85(1 Suppl):129s–132s.
- Hunt LW. Recent observations in serum sickness. JAMA. 1932 Sep 10;99(11):909–912.
- Beilory L. Clinical complications of heterologous antisera administration. J Wilderness Med. 1991 May;2(2):127–139.
- Weigle WO, Dixon FJ. Relationship of circulating antigen-antibody complexes, antigen elimination, and complement fixation in serum sickness. Proc Soc Exp Biol Med. 1958 Oct;99(1):226–231.
- Germuth FG Jr. A comparative histologic and immunologic study in rabbits of induced hypersensitivity of the serum sickness type. J Exp Med. 1953 Feb 1;97(2):257–282.
- Guttmann A, Krasnokutsky S, Pillinger MH, Berhanu A. Pegloticase in gout treatment—safety issues, latest evidence and clinical considerations. Ther Adv Drug Saf. 2017 Dec;8(12):379–388.
- Lipsky PE, Calabrese LH, Kavanaugh A, et al. Pegloticase immunogenicity: The relationship between efficacy and antibody development in patients treated for refractory chronic gout. Arthritis Res Ther. 2014 Mar 4;16(2):R60.
- Gupta S, Lau K, Harding CO, et al. Association of immune response with efficacy and safety outcomes in adults with phenylketonuria administered pegvaliase in phase 3 clinical trials. EBioMedicine. 2018 Nov;37:366–373.