The trial’s primary outcome was the estimated average treatment effect, defined as the difference in mean Disease Activity Score 28 with C-reactive protein (DAS28-CRP) among patients receiving adalimumab vs. tofacitinib at three and nine months after initiating treatment.
Research Summary
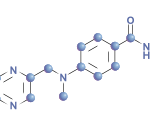
Deakin et al. examined 842 patients in the OPAL Rheumatology dataset. Patients were 18 years or older, had RA, were biologic or targeted synthetic DMARD naive and had at least six months of treatment with a conventional synthetic DMARD. Patients were excluded if they didn’t have at least one component of the DAS28-CRP recorded at baseline and at three and nine months. Most patients were women in their mid-to-late 50s. They were treated with 40 mg of subcutaneous adalimumab every 14 days or 5 mg of tofacitinib by mouth twice daily.
The estimated average treatment effect was -0.2 (95% confidence interval [CI], -0.4 to -0.03) at three months and -0.03 (95% CI, -0.2 to 0.1) at nine months. This translated to a “modest but statistically significant reduction in DAS28-CRP at three months” for patients receiving tofacitinib compared with those receiving adalimumab.3 There was no difference between drugs at nine months. Of note, three months of treatment with either drug led to clinically relevant average reductions in mean DAS28-CRP. This was consistent with previous noninferiority findings concerning for tofacitinib and adalimumab in a 2017 RCT.6
‘This study contributes data on the effectiveness of adalimumab & tofacitinib as used in everyday clinical practice in patients with RA who were DMARD naive & shows that patients respond well to either medicine.’ —Dr. Deakin
Implications
Dr. Deakin was kind enough to share her take on the clinical implications of her fascinating research.
The Rheumatologist (TR): What should practicing rheumatologists take away from these findings?
Dr. Deakin (CD): Both adalimumab and tofacitinib were effective and led to substantial reductions in disease activity at the three-month and nine-month follow-up time points, but tofacitinib led to slightly lower levels of disease activity at three months.
TR: How do these findings inform clinical practice?
CD: There are few studies comparing specific biologic and targeted synthetic DMARDs head to head. This study contributes data on the effectiveness of adalimumab and tofacitinib as used in everyday clinical practice in patients with RA who were biologic or targeted synthetic DMARD naive and shows that patients respond well to either medicine. This information may be useful if there are other circumstances to consider when selecting a biologic or targeted synthetic DMARD.