Unbeknownst to her, it was a patient who inspired David T. Felson, MD, MPH, to take up the challenge of rheumatology. In the late 1970s, Dr. Felson, then a resident at Case Western University Hospitals in Cleveland, was treating an older woman with arthritis who said to him, “I don’t know why you like helping me with my arthritis so much—you really can’t accomplish anything.”
“That statement was actually pretty insightful on her part,” he now reflects, because it pointed out one of the reasons why rheumatology was so challenging. Although rheumatologists did have some effective therapies for treating their patients, “that was before we had many of the newly available biologics,” he notes. His patient’s remark solidified his fascination for establishing relationships with patients and helping them work on their chronic illness problems.
The landscape of treatment armamentaria in rheumatic diseases has changed dramatically since that time, and Dr. Felson’s work over the past three decades has been critical to those advances. He has consistently collaborated with other disciplines—notably, epidemiologists in cardiology and oncology—to steer clinical measurement in rheumatology to new useful heights. Providing alignment of outcome measures, for example, has in turn allowed his bench research colleagues to measure the effectiveness of treatments.
Currently section chief of the clinical epidemiology research and training unit in the department of medicine at Boston Medical Center, and principal investigator of a Boston University (BU) NIH/NIAMS multidisciplinary clinical research grant, he is “one of a relatively small number of rheumatologists who are also first-class epidemiologists and clinical researchers,” says Michael C. Nevitt, PhD, MPH, a colleague and professor of epidemiology and biostatistics at the University of California San Francisco (UCSF) Medical School. “He is capable of doing large-scale population studies focusing on diseases that require clinically sophisticated and highly technical measurements to make advances in the field.”

Along the way, Dr. Felson has mentored a wide range of investigators who now contribute their insights not just to rheumatology but to other disciplines as well. Liana Fraenkel, MD, MPH, associate professor of medicine in the section of rheumatology of the department of internal medicine at Yale School of Medicine in New Haven, Conn., is one of those who benefitted from training with Dr. Felson. “His greatest contribution,” she says, “is that he formalized how to measure outcomes in rheumatoid arthritis trials, which enabled us to compare results across different trials.”
Social Sciences Background
Dr. Felson had planned on becoming a historian when he entered Harvard in 1970 as a National Merit Scholar. However, he also excelled in science, and “there weren’t any jobs in history,” he quipped during a phone interview, so he took a double major in history and biochemistry as an undergraduate. His father helped him get a summer job in a hospital physical therapy department, and it was then that Dr. Felson discovered that he “really loved interacting with patients—so that was what triggered my choice to go into medicine,” he says. He developed an interest in rheumatology as a Johns Hopkins University medical student during his rotation at the Good Samaritan Rheumatic Disease Unit founded by Mary Betty (“Marty”) Stevens, MD. It was an interest that strengthened later during his residency at Case Western University Hospitals in Cleveland, where he trained with Irving Kushner, MD.
By the time he had finished his residency, Dr. Felson notes that he was, indeed, much more attracted to the clinical than the laboratory science aspects of rheumatology. “Since I came from a social sciences background, it was more natural for me to go into epidemiology and public health and not bench science,” he explains. He headed to Boston University School of Medicine for a clinical and research fellowship.
Encouraged by his mentor, Robert F. (Bob) Meenan, MD, MPH, MBA, developer of the Arthritis Impact Measurement (AIM) scale, Dr. Felson began outreach to the investigators of the Framingham Heart Study. Started in 1948, the study had been tracking heart-disease measures for over three decades, but Meenan and Felson both realized there was an opportunity to begin to study arthritis in a community-based sample. This had not been done before, but many of the senior epidemiologists “had their doors open to me,” says Dr. Felson. His mentoring in epidemiology then began in earnest. “I relied very heavily on people from the methodology world [such as his long-time collaborator, statistician Jennifer J. Anderson, PhD] and not from the arthritis world,” he recalls. “I realized,” Dr. Felson now says, “that having expertise in epidemiologic methodologies would help provide insights into rheumatic disease problems.”
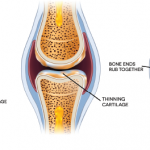
Investigators in the Framingham Study made useful suggestions as he struggled with designing measurements to assess arthritis in the cohort. The collaborations have yielded decades of insight into the prevalence, onset and progression of osteoarthritis (OA).1-3 The collaborations also created opportunities for his heart research colleagues. “They realized that they had been told by many heart-study participants that they were suffering from arthritis, so that was a big surprise to them as well,” he says.
It was Dr. Felson’s own experience with both clinical research and methodology that led him to encourage his trainees over the years to acquire expertise in both arenas. “A person pursuing research in rheumatology has to bring both pieces—the clinical and the methodological expertise—to the table to make the biggest contributions to help improve the lives of those with arthritis,” he asserts. His embrace of those twin components has yielded critical knowledge for the field.
“Dr. Felson’s scientific vision is critical to advancing our clinical knowledge of OA,” says Chhanda Dutta, PhD, chief of the clinical gerontology branch in the division of geriatrics and clinical gerontology at the National Institute on Aging (NIA) in Bethesda, Md. He is the only nonbiomedical researcher to have received the Henry J. Kunkel Young Investigator Award from the ACR.

An Extraordinary Mentor
As a mentor, Dr. Felson has consistently guided and nurtured his trainees. Dr. Fraenkel noted that Dr. Felson follows an open-door policy. “We always felt comfortable barging in on him, whether it was to ask a relatively straightforward methodological question or to engage in more weighty conversations regarding research strategies or career planning.”
That was also the experience for Shreyasee Amin, MD, CM, MPH, associate professor of medicine in the division of rheumatology in the department of internal medicine at the Mayo Clinic in Rochester, Minn, when she trained at BU with Dr. Felson. “He was always available to me, but he was not directive,” she says. “He would allow me to work and think through ideas and provide appropriate guidance.” Dr. Amin had originally planned on a two-year research fellowship at BU, but stayed for almost four because of the wealth of opportunities offered her. She also benefitted from Dr. Felson’s interdisciplinary approach to research: “Dr. Felson’s view was that collaboration outside of rheumatology and even outside of epidemiology brings more information and richness to the research.” Working at BU with Dr. Felson, she collaborated with biomechanical engineers at the New England Research Institute to study gait analysis. She is currently involved in osteoporosis research that pairs her with endocrinologists to understand the hormonal and biomarkers aspects of the disease, as well as with NASA scientists to ferret out the interplay of exposure to microgravity and long-term risk for fracture. She has also continued her ongoing collaborations with Dr. Felson’s group at BU examining risk factors for cartilage loss as determined by MRI and knee symptoms in those with knee OA.
“There is no shortage of brilliant professors in academic medicine, but extraordinary mentors are scarce,” wrote Dr. Fraenkel in a 2007 nomination letter to the Teaching Awards Committee at BU School of Medicine. Even more notable, in Dr. Fraenkel’s mind, was Dr. Felson’s belief in the success of his trainees. Toward the end of her fellowship, she developed a research interest outside of Dr. Felson’s niche. (She now concentrates on medical decision-making from the patient and clinician perspective.) “David encouraged me to pursue my research agenda and gave me the protected time, advice, and support I needed to learn new disciplines and to foster collaborations with relevant experts outside of Boston University.”
Dr. Felson was awarded the inaugural Robert Dawson Evans Research Mentoring Award at BU in 2007.
Forging New Territories
Dr. Felson has consistently applied his multidisciplinary bent to exploring key questions in rheumatic diseases. In 1998, Dr. Dutta of the NIA recalls, he and Dr. Nevitt approached the institute with a concept for the Multicenter Osteoarthritis Study (MOST).4 “At that time,” she says, “there was a lot of discussion in the OA field about the discrepancy between radiographic changes in the knee and the symptomatology reported by patients. There was also limited availability of information on modifiable risk factors for the onset and progression of knee OA. The innovative aspect of the MOST project was that it sought to address key knowledge gaps in the OA field through the use of X-rays and MRIs, in a prospective longitudinal study design.” The NIA issued grant awards to the MOST study in 2001 and follow up of the MOST cohort is ongoing.
In the late 1990s, Dr. Felson saw an opportunity to expand investigations to Asia. Through his colleague Dr. Nevitt and other colleagues at UCSF, linkage with a Chinese investigator, Ling Xu, based at the Peking Union Medical College in Beijing, was established. The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) funded a study to compare knee, hip, and hand OA among Chinese to Caucasians in the Framingham study and the UCSF Study of Osteoporotic Fractures. (Listen to Dr. Felson discuss the study.)
Dr. Nevitt recalls the experience, which included six or seven trips to China, as an “amazing, fun, and challenging experience.” He says, “we had some great collaborators in China who already had experience doing this kind of study with osteoporosis. I think that David was really excited by this project: being able to address a question that he had posed in review articles many years before about distribution of OA in various countries and ethnic groups.”
Taking into account cultural nuances challenged the research team, says Dr. Nevitt, as they strived to develop and translate existing questionnaires that would have relevance in the Chinese population. All in all, says Dr. Nevitt, the Beijing study remains one of the highlights of his collaborations with Dr. Felson.5 (They are also co-investigators on the MOST [Multicenter Osteoarthritis Study].) “[The Beijing study] was a lot of fun, and David made it a wonderful experience,” he recalls.
A longstanding interest in meta-analysis has also been a key factor in Dr. Felson’s involvement with the ACR’s efforts to establish definitions of remission in RA for clinical trials. “I was impressed with the cancer world,” he says, “which seemed to have figured out how to standardize indicators. They have actual numbers of how many people with disease go into remission, and what treatments work. We didn’t have anything like that in rheumatology.” He helped to create an international committee of participants to establish a provisional definition of disease remission in RA to be used in clinical trials.6
Currently, Dr. Felson’s work is multipronged. He holds a part-time appointment at the University of Manchester in the U.K., directs the Clinical Epidemiology Research Training Unit at BU, and is now involved in studies of foot disorders in the elderly, and of back pain and its impact on the elderly. As the ongoing principal investigator in the Framingham Osteoarthritis Study, he also continues to publish on findings about hand OA in the general population.7 In his free time, he enjoys traveling and singing.
The Clinical Epidemiology Research Training Unit is engaged in a broad spectrum of research, ranging from studies of gout, OA, work disability prevention, outcome measures in rheumatoid arthritis, biomarker studies in vasculitis, and genome-wide association studies of pain and gout. “Dr. Felson has amassed an amazing group of people (including epidemiologists, biostatisticians, programmers, physicians, and other healthcare professionals) who grapple with the nitty-gritty of very advanced methodology here,” says Tuhina Neogi, MD, PhD. She began training in 2003 supported by an Arthritis Foundation grant. In addition to being a research fellow with the NIH-funded Clinical Research Training (CREST) program that supports formal research training through course work, she also benefitted from the unit’s infrastructure that provided the opportunity for a true apprenticeship: “the ability to immerse oneself in the nuts and bolts of research,” she says. Now, as an associate professor of medicine, she is challenged daily by the nuanced discussion and debate emblematic of the unit’s investigators.
The photograph of the Clinical Epidemiology Research and Training Unit, with a group of trainees surrounding a beaming Dr. Felson, attests to the vibrancy of the program he continues to nurture. Recalls Dr. Fraenkel, “I have been with David both when he has been on stage to receive awards celebrating his success as a researcher and when he is watching his fellows present at national meetings, and the smile on his face is always much larger when his trainees are on the stage.”
Gretchen Henkel writes the “Metrics in Rheumatology” series.
Timeline
1978 – Earns his MD from the Johns Hopkins School of Medicine
1981 – Completes internship and residency in internal medicine at Case Western University Hospitals
1984 – Completes clinical and research fellowship at Boston University School of Medicine
1984 – Earns MPH at Boston University School of Public Health
1984 – Becomes assistant professor of medicine and public health (epidemiology) at Boston University School of Medicine
1989 – Becomes associate professor of medicine and public health (epidemiology and biostatistics) at Boston University School of Medicine
1994 – Becomes professor of medicine and epidemiology at Boston University Schools of Medicine and Public Health
2008 – Becomes professor of medicine and public health at the University of Manchester (part time)
References
- Felson DT, Naimark A, Anderson JJ, et al. The prevalence of knee osteoarthritis in the elderly. The Framingham Knee Osteoarthritis Study. Arthritis Rheum. 1987;30:914-918.
- Felson DT, Anderson JJ, Naimark A, et al. Obesity and knee osteoarthritis. Ann Int Med. 1988;109:18-24.
- Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: Methodological issues in the study of disease and physical disability.” Amer J Public Health. 1990; 80:945-949.
- Zhang Y, Nevitt M, Niu J, et al. Fluctuation of knee pain and changes in bone marrow lesions, effusions, and synovitis on magnetic resonance imaging. Arthritis Rheum. 2011;63:691-699.
- Felson DT, Nevitt MC, Zhang Y, et al. High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasians. Arthritis Rheum. 2002;46:1217-1222.
- Felson DT, Smolen JS, Wells G, et al. American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum. 2011;63: 573-586.
- Haugen IK, Englund M, Aliabadi P, et al. Prevalence, incidence and progression of hand osteoarthritis in the general population: The Framingham Osteoarthritis Study. Ann Rheum Dis. 2011;70:1581-1586.