The diversity of pulmonary lesions in IgG4-RD broadens significantly the differential diagnosis that the rheumatologist must consider when evaluating a patient with lung problems. Nodular lesions may represent lung tumor, an opportunistic infection, granulomatosis with polyangiitis (Wegener’s granulomatosis), and other entities—but also IgG4-related lung disease. Similarly, ground-glass opacities may indicate fluid overload, viral infection, alveolar hemorrhage, bronchoalveolar carcinoma, and other diagnoses, including IgG4-related lung disease. Even honeycombing, part of the advanced stage of interstitial lung disease and nonspecific or usual interstitial pneumonitis that characterizes a broad swath of rheumatologic disease that includes rheumatoid arthritis, systemic sclerosis, inflammatory myopathies, and antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis occurring in the setting of antimyeloperoxidase ANCA, may also be the result of IgG4-RD. Finally, confronted with the striking thickening of the bronchovascular bundle that can be caused by IgG4-RD, the rheumatologist must also consider lymphomatoid granulomatosis, multicentric Castleman’s disease, and sarcoidosis, among others.
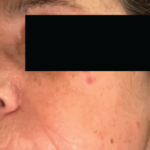
Positron emission tomography (PET) with CT can be useful to determine the extent of disease and may also be helpful to gauge disease activity and response to treatment. Our patient underwent a PET/CT that revealed unanticipated findings in the lung, demonstrating bronchiectasis, ground glass opacities, and pulmonary nodules (see Figure 5, at right) in addition to showing increased tracer uptake in his parotid glands and lymph nodes.
What Is the Treatment for IgG4-RD?
Glucocorticoids are the first-line treatment for IgG4-RD. Many cases require aggressive and immediate treatment to prevent organ dysfunction and failure. However, other disease manifestations (e.g., IgG4-related lymphadenopathy) may remain indolent and relatively asymptomatic for years.14 Therefore, the treatment regimens must be individualized for each patient. One approach to the use of glucocorticoids is to treat patients initially with prednisolone at a dose of 0.6 mg per kilogram of body weight per day for two to four weeks and then to taper the steroids over a period of three to six months.15 Some investigators, wary of the long-term complications of glucocorticoids, have aimed to discontinue these agents after three months.16 Agents such as azathioprine, mycophenolate mofetil, and methotrexate have been employed as potential glucocorticoid-sparing agents or remission–maintenance drugs, but their true efficacy in these roles is unclear.
For patients with IgG4-RD that is refractory to glucocorticoids, patients that are unable to taper below a desired dose, or patients with recurrent IgG4-RD, B-cell depletion with rituximab may represent a promising approach to treatment.17 Patients treated with rituximab have generally demonstrated prompt clinical and serological responses, with the ability to taper glucocorticoids rapidly and a swift decline in serum IgG4 concentrations. Moreover, the decline in serum IgG4 concentrations appears to be isolated, targeting this IgG subclass alone while leaving the concentrations of IgG1, IgG2, and IgG3 stable.18 This finding suggests that one potential mechanism of rituximab’s efficacy in IgG4-RD is through interference with the repletion of short-lived plasma cells that are producing IgG4 in this condition. Additional studies of this hypothesis are required, however, and an ongoing clinical trial will investigate these concepts further.