BALTIMORE—Many rheumatologists know that vasculitis can rapidly lead to morbidity and mortality for afflicted patients. Thus, understanding the advances in care for vasculitis is key to preventing patient suffering and saving lives.
BALTIMORE—Many rheumatologists know that vasculitis can rapidly lead to morbidity and mortality for afflicted patients. Thus, understanding the advances in care for vasculitis is key to preventing patient suffering and saving lives.
At the 18th Annual Advances in the Diagnosis & Treatment of the Rheumatic Diseases, held May 13–14 at Johns Hopkins School of Medicine, Baltimore, Brendan Antiochos, MD, assistant professor of medicine, Division of Rheumatology, Johns Hopkins School of Medicine, and assistant director of the Johns Hopkins Vasculitis Center, discussed important topics in vasculitis. He addressed new medications for anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis and giant cell arteritis (GCA), tapering of glucocorticoids in patients with vasculitis and issues related to vaccination against SARS-CoV-2 in patients with vasculitis, particularly those receiving B cell-depleting therapy.
Avacopan
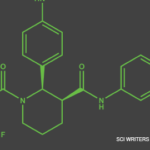
Dr. Antiochos began by discussing the ADVOCATE trial, a large, international, randomized clinical trial comparing avacopan (a C5a receptor inhibitor) with prednisone in patients with ANCA-associated vasculitis who were receiving either cyclophosphamide plus azathioprine, or rituximab.1
Dr. Antiochos explained that the C5a receptor can be found on myeloid cells and that activation of this receptor helps recruit these cells to sites of injury or inflammation. Avacopan is designed to block the C5a receptor and prevent such recruitment without affecting the formation of the membrane attack complex, which is a product of the complement system and helps protect against certain pathogens.
In 2014, researchers tested a mouse model of necrotizing and crescentic glomerulonephritis mediated by anti-myeloperoxidase antibodies, as would be seen in ANCA-associated vasculitis. They found oral administration of avacopan—called CCX168 at that time—prevented anti-myeloperoxidase-induced necrotizing and crescentic glomerulonephritis in mice expressing human C5aR/CD88.2
In the ADVOCATE trial, patients were randomized to receive either 30 mg of avacopan twice daily or an oral prednisone taper, with background therapy of either cyclophosphamide induction followed by azathioprine maintenance or rituximab. The main characteristics of study participants were patients who were newly diagnosed and had seropositive ANCA-associated vasculitis. The majority had renal disease and had been treated with rituximab. The study’s primary end points were clinical remission at week 26, with a Birmingham Vasculitis Activity Score (BVAS) of 0 and no steroids for at least four weeks before week 26, and sustained remission at weeks 26 and 52, with no glucocorticoids for at least four weeks before week 52.
The results: Avacopan proved noninferior to the oral prednisone taper for clinical remission at week 26 and was superior to the oral prednisone taper for sustained remission at week 52. Roughly 10% of the avacopan patients experienced a relapse of disease at week 52 compared with about 20% of those in the oral prednisone taper group. In total, patients in the avacopan group received about one-third less total prednisone than those in the oral prednisone taper group. An additional exciting finding described by Dr. Antiochos was that renal function in patients treated with avacopan continued to improve throughout the study.1
Dr. Antiochos pointed out that patients treated with rituximab in the study were given this medication only as induction—a dose of 375 mg per meter squared of body surface area, given weekly for four weeks. No maintenance dosing was given at six months after induction, potentially increasing the risk of relapse. Also, the glucocorticoid taper was rapid, with tapering completed by week 21, faster than in current clinical practice. Finally, Dr. Antiochos explained that patients in the avacopan arm of the trial received some glucocorticoids. Thus, this study was not truly a glucocorticoid-free intervention.
Nevertheless, the findings of the ADVOCATE trial and the approval of avacopan by the U.S. Food & Drug Administration (FDA) are notable developments and warrant further exploration of the appropriate use of this medication in clinical practice.
The findings of the ADVOCATE trial & the approval of avacopan by the FDA are notable developments & warrant further exploration of the appropriate use of this medication in clinical practice.
Managing GCA
Next, Dr. Antiochos discussed mavrilimumab and GCA. Mavrilimumab is a human monoclonal antibody that inhibits the human granulocyte macrophage colony-stimulating factor receptor (GM-CSF), which promotes the differentiation, activation and survival of myeloid cells. Because upregulation of GM-CSF and its receptor have been found in temporal artery biopsies in patients with GCA, biologic plausibility exists for the use of mavrilimumab to treat GCA.3
In a phase 2, randomized, double-blind, placebo-controlled clinical trial on the efficacy and safety of mavrilimumab, patients with GCA, aged 50–85 and new or relapsing active disease were randomized to receive either mavrilimumab or placebo. Both groups received background treatment with a 26-week prednisone taper. The primary end point of this study was time to first disease flare as defined by erythrocyte sedimentation rate (ESR) levels of >30 mm/hr or C-reactive protein (CRP) levels of >1 mg/dL, along with clinical signs and symptoms of vasculitis activity or imaging evidence of vasculitis activity.
Results: Mavrilimumab proved superior to placebo for time to flare by week 26 and sustained remission in patients with GCA who were treated with a background, 26-week prednisone taper. The medication also appeared safe, with few reported adverse events overall. Dr. Antiochos noted that patients who experienced a disease flare with mavrilimumab demonstrated elevated acute phase reactants. This finding contrasts with what is seen in patients with GCA who are treated with tocilizumab, which suppresses inflammatory markers, such as CRP, making it challenging to use such markers to evaluate if a patient is experiencing disease relapse.
Next, Dr. Antiochos addressed the GUSTO study, a proof-of-concept trial evaluating what happens to patients treated with intravenous pulse steroids at the onset of disease and then with tocilizumab monotherapy without ongoing steroids. Enrolled patients had new-onset disease (i.e., diagnosis within four weeks or less) with CRP levels of >25 mg/L, diagnosis proved with biopsy or magnetic resonance/positron emission tomography imaging, and glucocorticoids given for less than 10 days at a maximum dose of 60 mg of prednisone daily. In the study, patients were treated with 500 mg of intravenous (IV) methylprednisolone daily for three days, one dose of IV tocilizumab measured at 8 mg/kg of body weight, and then 162 mg of subcutaneous tocilizumab given weekly for 52 weeks.
The findings: Patients did better than expected. Although only 25% of patients were in remission after 31 days, 78% were in remission by week 24, with 72% remaining relapse free through week 52. However, one patient suffered the onset of anterior ischemic optic neuropathy, one of the most feared complications of disease due to its effects on vision.4 Thus, Dr. Antiochos said his takeaway from this proof-of-concept study was that the glucocorticoid course used in this trial was likely too short, but that current tapering protocols used in clinical practice may represent overtreatment.
COVID-19
Lastly, Dr. Antiochos discussed several clinical pearls related to preventing COVID-19 in patients with vasculitis who are receiving, or will receive, therapy with B cell-depleting agents, such as rituximab.
Given the data on this subject, he advised the administration of SARS-CoV-2 vaccine booster shots be scheduled when B cells have reconstituted in patients treated with rituximab. Also, two patients with ANCA-associated vasculitis who, despite complete B cell depletion after treatment with rituximab, reportedly demonstrated an antibody response to a booster vaccination. These two patients received Johnson & Johnson as their initial vaccine and subsequently the Moderna or Pfizer booster series, perhaps demonstrating improved immunogenicity with combining different types of vaccines.5
Finally, Dr. Antiochos reminded the audience that in December 2021 the FDA issued an emergency use authorization for Evusheld (tixagevimab and cilgavimab). This authorization is for pre-exposure prophylaxis of individuals who are moderately to severely immunocompromised due to a disease or medication and may not mount an adequate immune response to COVID-19 vaccination.
Jason Liebowitz, MD, completed his fellowship in rheumatology at Johns Hopkins University, Baltimore, where he also earned his medical degree. He is currently in practice with Skylands Medical Group, N.J.
References
- Jayne DRW, Merkel PA, Schall TJ, et al. Avacopan for the treatment of ANCA-associated vasculitis. N Engl J Med. 2021 Feb 18;384(7):599–609.
- Xiao H, Dairaghi DJ, Powers JP, et al. C5a receptor (CD88) blockade protects against MPO-ANCA GN. J Am Soc Nephrol. 2014 Feb;25(2):225–231.
- Corbera-Bellalta M, Alba-Rovira R, Muralidharan S, et al. Blocking GM-CSF receptor α with mavrilimumab reduces infiltrating cells, pro-inflammatory markers and neoangiogenesis in ex vivo cultured arteries from patients with giant cell arteritis. Ann Rheum Dis. 2022 Apr;81(4):524–536.
- Christ L, Seitz L, Scholz G, et al. A proof-of-concept study to assess the efficacy of tocilizumab monotherapy after ultra-short glucocorticoid administration to treat giant cell arteritis-the GUSTO trial [OP0061]. Ann Rheum Dis. 2021;80:33.
- Kant S, Azar A, Geetha D. Antibody response to COVID-19 booster vaccine in rituximab-treated patients with anti-neutrophil cytoplasmic antibody-associated vasculitis. Kidney Int. 2022 Feb;101(2):414–415.