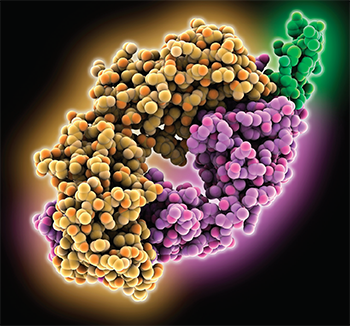
Computer model showing the
structure of the rituximab fab light chain (yellow) and heavy chain (purple) complexed with the B-lymphocyte antigen CD20 (green).
LAGUNA DESIGN / Science Source
Researchers sought to identify predictors of patients with anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) who took rituximab for maintenance had a better sustained remission rate through 60 months than those taking azathioprine, according to the latest results from the maintenance of remission using rituximab in systemic ANCA-associated vasculitis (MAINRITSAN) trial, a prospective, randomized trial by the French Vasculitis Study Group.1
Rituximab proved superior to azathioprine for remission maintenance through 28 weeks, according to earlier findings from the trial, and rituximab’s relapse rate remained better through week 60.
“Rituximab had a superior post-treatment efficacy than azathioprine at maintaining remissions of ANCA-associated vasculitides over 60 months,” says Benjamin Terrier, MD, PhD, the lead author and consultant of internal medicine at Paris Descartes University, Paris, France. “Rituximab had superior benefit and no safety differences with azathioprine.”
Anisha Dua, MD, MPH, director of the Vasculitis Center at the University of Chicago, did not participate in the study, but she says the results affirm rituximab should play a significant role in maintenance.
“These findings support the efficacy of rituximab 500 mg infusions every six months as superior to azathioprine at 60-month follow-up in new and relapsing patients with GPA and MPA,” she says, referring to granulomatosis with polyangiitis and microscopic polyangiitis, respectively. “The side effect profile was comparable, but the rate of relapse was lower in the rituximab treated group. In practice, the implications are that we should really consider using rituximab therapy for maintenance in our patients with GPA and MPA.”
The experts note that an increased number of patients taking rituximab suffered major relapses after the 28-week mark—more than in the azathioprine group—which they say underscores the need to fine-tune maintenance strategies for the disease, including trying to identify patients for whom longer treatment durations may prove beneficial.
Nearly the same number of patients suffered severe infections in each group.
The Study Details
In the trial, researchers enrolled 115 patients with newly diagnosed or relapsed granulomatosis with polyangiitis, microscopic polyangiitis or renal-limited ANCA-associated vasculitis. They were all in complete remission after being treated with glucocorticoids and cyclophosphamide.

Dr. Dua
Patients were randomized to either receive rituximab, with two early doses of 500 mg and then doses at Months 6, 12 and 18, or azathioprine, with 2 mg/kg per day for 12 months, then 1.5 mg/kg per day for six months, then 1 mg/kg per day for four months. Decisions on prednisone dose tapering and stopping prednisone after 18 months were left to the investigators at each center. Prophylaxis with co-trimoxazole was recommended for patients with fewer than 250 CD4-positive T cells per mm3.
Investigators reported earlier that at 28 months, 17 patients in the azathioprine group suffered a major relapse; that is, a reappearance or worsening of the disease with one major organ involved or some life-threatening manifestation. That compared to just three major relapses in the rituximab group. Nine patients in the azathioprine group suffered a minor relapse.
Between months 28 and 60, 11 patients suffered a major relapse in the azathioprine group among those who’d been major relapse free, while 13 in the rituximab group suffered a major relapse. Three and seven patients suffered minor relapses, respectively.
At 60 months, the major relapse-free survival rate was 49.4% in the azathioprine group and 71.9% in the rituximab group (P=0.003). The completely relapse-free rate was 37.2% and 57.9% (P=0.012), respectively.
Nearly the same number of patients suffered severe infections in each group—16 for azathioprine and 15 for rituximab—but there were more instances of severe infection in the rituximab group (31) compared with the azathioprine group (20). Most of the infections were respiratory, and those were also more frequently seen in the rituximab group, including 10 cases of bronchitis compared to just one in the azathioprine group.
Three patients developed Pneumocystis jiroveci pneumonias, with none of the patients on prophylaxis at the time of infection—one because it had been discontinued, one due to allergy and poor compliance with a substitute, and another due to allergy. Experts say this highlights the need for clinicians to emphasize prophylaxis to their patients.
An analysis showed those on rituximab went 12.6 more months without a relapse or toxicity than those taking azathioprine (P<0.001).
Dr. Terrier says that despite rituximab’s superiority over five years, the increased number of relapses in the group shows the need to continue to improve maintenance treatment.
“Rituximab could delay rather than abrogate relapses,” he says.
Relapse Risk Factors
Among all patients, those with antiproteinase3 (PR3) ANCA antibodies were at an increased risk of relapse compared with those with anti-myeloperoxidase (MPO) ANCA or no ANCA antibodies, investigators found (hazard ratio [HR]=2.18; P=0.012).
Researchers found ANCA status and B cell counts to be telling. In the azathioprine group, researchers found 22 of the 27 patients were ANCA positive at relapse. In the rituximab group, none of the three patients who suffered a major relapse before Month 28 had CD19 B cell reconstitution, but two of them were ANCA positive at relapse. But after that, 12 of the 13 with a major relapse were ANCA positive at relapse, and they all showed CD19 B cell reconstitution.
“Patients with PR3-ANCA at baseline and with ANCA that remain or become positive during follow-up are at high risk of relapse,” Dr. Terrier says. He said no data are yet available to guide clinicians on whether these patients should be treated for the same duration as other patients and simply be closely monitored, or whether they should be treated for a longer period of time than patients who remain negative for PR3-ANCA.
“Overall, the main concern from these results is clearly the need to better identify patients with high-relapse risk [who] could benefit from longer treatment, and efforts are currently being made to optimize treatment strategy,” he says.
These efforts are now underway. In the United Kingdom, in the rituximab vs. azathioprine as therapy for maintenance of remission for anti-neutrophil cytoplasm antibody-associated vasculitis (RITAZAREM) trial, researchers are evaluating the efficacy of a higher rituximab dose—1 g every four months over 20 months—compared with azathioprine. And in MAINRITSAN3, investigators are looking at the benefit-to-risk ratio of continuing rituximab for 18 more months than the duration used in MAINRITSAN.
Dr. Dua says the relapses seen in each group were not necessarily surprising, with those in the azathioprine group beginning to relapse in the first year after drug discontinuation and rituximab patients starting to experience major relapse 18–24 months after the last infusion. She says it is also important to note the rituximab-treated patients who suffered major relapses saw reconstitution of their B cells at the time of relapse.
“Of course, it would be wonderful to see the rituximab group stay relapse free throughout the length of this follow-up—60 months,” she says. “However, the results reflect the mechanisms of action of the drugs used.”
Questions still facing researchers and clinicians include whether higher doses of rituximab would be just as safe but more effective, whether the duration of rituximab treatment should be lengthened and whether such markers as seroconversion, ANCA titers and B cell population could signal windows of opportunity to redose or increase dosage for longer relapse-free periods. Upcoming studies could help answer these questions, Dr. Dua says.
“Other questions not specific to rituximab dosing include whether low doses of prednisone—even though we are trying to minimize steroid exposure—might enable select patients to stay in remission longer,” she says. “Are there other biomarkers that can help us identify disease earlier, or features—genetic, clinical, serologic, pathologic or otherwise—specific to patients that can help us to identify the precise medication that will be most effective and best tolerated for a specific patient?”
Thomas R. Collins is a freelance writer living in South Florida.
Reference
- Terrier B, Pagnoux C, Perrodeau É, et al. Long-term efficacy of remission-maintenance regimens for ANCA-associated vasculitides. Ann Rheum Dis. 2018 Aug;77:1150–1156.