On Nov. 1, the Centers for Medicare & Medicaid Services (CMS) issued the CY2023 Medicare Physician Fee Schedule Final Rule. The CMS finalized many policies from the July proposed rule, including a 4.5% decrease in the conversion factor, delayed implementation of split/shared visit coding requirements, continuation of telehealth flexibilities through 2023 and adoption of five-minute pre- and post-service times for musculoskeletal ultrasound as recommended by the American Medical Association’s Relative Value Scale Update Committee (RUC).
Conversion Factor
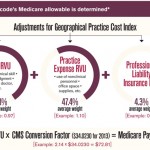
The final rule codified the conversion factor of $33.06. This represents a $1.55 decrease and accounts for budget-neutrality statutory requirements and the sunset of the 3% supplemental COVID-19 payments. The conversion factor is a critical factor in the reimbursement formulation. Therefore, the significant decrease in conversion factor will negatively impact every code and decrease reimbursement for all services and specialties. With other organizations, the ACR is co-leading advocacy efforts to ask Congress to avert these detrimental cuts before the end of the current Congress.
Geographic Practice Cost Indices
Every three years, the CMS must review and, if necessary, readjust the Geographic Practice Cost Indices (GPCI) used in the overall reimbursement algorithm. The GPCI reflects the geographic variations in the cost to provide care. For the CY23 Final Rule, the CMS will use the 2017–20 Bureau of Labor Statistics Occupational Employment Statistics to determine wage data and the 2015–19 American Community Survey to determine local practice expenses.
Evaluation & Management Services
The final rule continues to operationalize the updated evaluation and management (E/M) revaluation and documentation requirements that went into effect in January 2021. Following significant advocacy from the ACR and other organizations, the CY23 final rule delays the implementation of split/shared visits that would require visits to be billed by the practitioner who provides the substantive portion of the visit or more than half the time spent in the visit. Instead, providers will continue to choose history, physical exam, medical decision making or more than half the total practitioner time to determine the “substantive portion” of the visit.
Telehealth
At the onset of the public health emergency, the CMS issued broad flexibility for telehealth, including site-of-service requirements. In 2021, many of these options were included in a third category under the covered services to allow the continuation of telehealth services. The CY23 final rule reiterated the continuation of this flexibility through 2023. The CMS will use this time to evaluate which options should be made permanent in a post-pandemic telehealth environment. The ACR will engage with the CMS as it continues to envision telehealth after the public health emergency.