Gajus/shutterstock.com
In 2008, the American College of Rheumatology Workforce Study Advisory Group published a comprehensive rheumatology workforce analysis.1 It concluded:
Based on assessment of supply and demand under current scenarios, the demand for rheumatologists is expected to exceed supply in the coming decades. Strategies for the profession to adapt to this changing health care landscape include increasing the number of fellows each year, utilizing physician assistants and nurse practitioners in greater numbers, and improving practice efficiency.
Eight years later, our specialty faces the same intractable shortage. To put it simply, no number of additional rheumatologists can close our care, disease outcome and professional income gaps until we fundamentally change the way our practices function. We need to focus on improving the effectiveness, efficiency and profitability of rheumatic disease care and on redesigning our academic teaching programs to better prepare trainees for increasingly challenging real-world practice environments.
A Perspective Change
We can’t do better until we see it differently.

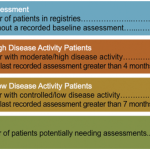
(click for larger image) Table 1: On-Time Assessment Rates*
*MBDA test data. Similar care gaps observed for other measures.
There have always been, and still are, exceptionally successful practices in rheumatology—and in other specialties managing chronic diseases.2 As a rule, however, rheumatologists provide physician-centric care one patient at a time, room to room, organized around each physician’s preferred appointment schedule. This is how we were taught, this is what we do, and this is what we have to change.
One exceptional rheumatologist and an ACR Master was Jacques Caldwell. He saw things differently: “I only do what only I can do.” His care teams saw 70+ patients a day and participated in many clinical trials, and yet his patients told him, “You are my only physician who has time for me when I need you.”3
From an income perspective, the ACR Workforce Study identified a minority of colleagues who take home two to three times the median rheumatology income.1 Unfortunately, income benchmarks for rheumatology are generally set at the median, potential trainees know these numbers, and we don’t compare favorably to other, more popular, specialties. What have these outliers figured out that the rest of us haven’t?
New Solutions Are Needed
The Rheumatoid Arthritis Practice Performance (RAPP) Project is a voluntary consortium of practicing rheumatologists founded in 2013 to improve our patient access, delivery of care and disease outcomes. Our primary focus is to provide accurate, on-time disease activity assessments and necessary treatments for our entire RA populations consistent with treat-to-target recommendations.4