GLENDALE, ARIZ.—Arizona is a microcosm of America’s challenges in reconciling the rheumatology workforce to growing patient demand, as quantified in the ACR’s Workforce Study of 2015.1 So it was timely this year for the Phoenix Rheumatology Association to sponsor its 1st Annual Strategic Training for Rheumatology Advanced Practice Clinicians Symposium. (Note: Advanced practice clinicians [APCs] is the preferred collective term for nurse practitioners [NPs] and physician assistants [PAs]).
Sixty-seven APCs from 22 states gathered in Glendale, Ariz., May 4–6, 2018, for a series of clinical lectures and more. Opening with an appraisal of the role that APCs play in helping close the current and evolving workforce gap, the curriculum included two interactive sessions orchestrated to begin building best practice concepts that may assist rheumatology practices with onboarding APCs and nurturing their careers in the field. The viewpoints and concerns of APCs, as well as qualitative and semi-quantitative information gathered in the symposium, may be of use to rheumatologists considering adding APCs to their operational structure.
The Workforce Shortage
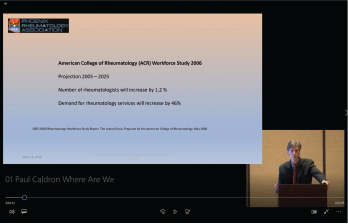
Dr. Caldron presented data from the ACR Workforce Study at the 1st Annual Strategic Training for Rheumatology Advanced Practice Clinicians Symposium.
In brief, the current deficit of 700 rheumatologists in the U.S. will expand to 4,100 by 2030. The specialty can anticipate a decrease of 31% in workforce concomitant with an increase of 138% in demand for services. Among the cited forces working against the workforce are the opportunity costs of a career in the specialty, retirement of the baby boom generation, effects of the male to female workforce gender transition, return of international medical graduates to their home countries and fellowship graduates seeking less than full-time work.2
Rheumatology-filled training positions increased between 2012 and 2016, but the anticipated 107 full-time equivalents from current training programs fall woefully short of replacing the more than 200 projected annual retirements. In this milieu, the hoped-for remedy to supplement practices with APCs would establish a ratio of APCs to rheumatologists at 1:10.
One medical practice, Arizona Arthritis and Rheumatology Associates (AARA), that has tapped into this resource over nearly 25 years approaches a ratio of 2:1. A universal strategy of this kind may mitigate the deficit substantially.
Multiple organizations are involved in efforts to leverage this APC lifeline. The ACR maintains its modular online curriculum for allied health professions and provides a consensus-developed curriculum for the training of APCs. In March, it announced a grant in support of in-service training for individual APCs. The Rheumatology Nurses Society (RNS) provides symposia geared synchronously to APCs and infusion nursing staff. The composite of literature specific to APCs in rheumatology, although thin, generally affirms the specialty as a compatible and effective niche for these professionals.3-6



