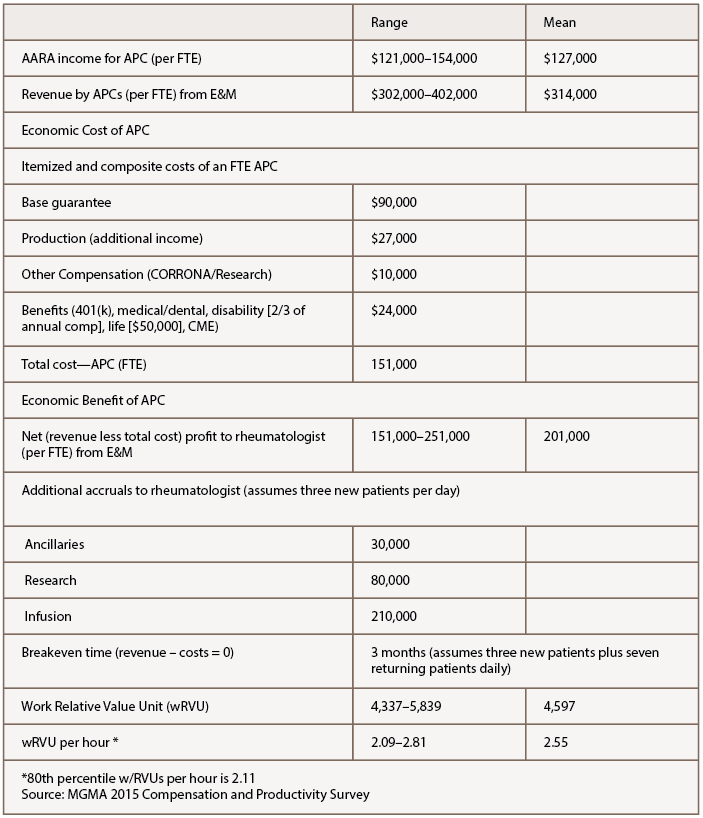
The APC’s impact on other remunerative streams in the practice, such as ancillary services, infusion services and clinical research, are also estimable and substantive. Typically, the breakeven point of employment wherein APC revenues cover APC costs is three months in AARA’s operational model, seeing three new patients and seven return visits daily. Within that model, the mean wRVU per hour is 2.55.
Participants in the symposium commented that understanding how their earnings are calculated transparently, what costs are attributed to them and what they produce for the practice would provide a sense of control and lower anxiety about their financial relationship with their rheumatologists and their organizations. De-identified benchmarking to their peers in all calculations helps with goal setting.
Models
In another interactive session of the symposium, the prevalence of several rheumatology APC working models was evaluated. Five NPs in attendance were working without a rheumatologist where state laws allow independent practice.
Within the group setting, a show of hands placed most of the remaining participants split equally between a shared patient panel model with a specific rheumatologist and being responsible for their own panel of patients. One participant characterized her group of four rheumatologists and three APCs as successfully interacting in a loose fashion without any preset team structure.
In the AARA model, APC activities mimic permanent fellows in rheumatology. The model generally satisfies the professional aspirations of the APCs, functions well in economic terms, is embraced by patients and the referral base, and accrues a workforce for the community not otherwise achievable with the current dearth in new graduate rheumatologists.
Participants from other practices commented that in their practices, some physicians were happy to have APC associates while others were resistant or had no interest in their utilization. One APC intent on a full career in rheumatology expressed interest in practice ownership by APCs with physicians, a model for which there is precedent.
Play It Again
A near 50% post-symposium response gave the Phoenix Rheumatology Association a composite 93% approval on the clinical presentations, and 97% would like to repeat the program in 2019. Venues geared for rheumatology APCs have a future and should play a role in promoting the rheumatology APC identity and expansion. Advancing the exploratory ideas of these motivated colleagues through structured study of APC utilization, clinical training and professional development should leverage this opportunity to mind the gap.