Patients with juvenile idiopathic arthritis (JIA) commonly experience ocular complications and vision loss. As uveitis activity increases, so does the risk for vision loss. A new study confirms that the use of immunosuppressive drugs is associated with a reduced risk of vision loss in patients with JIA-related uveitis.1 New data also indicate that the use of immunosuppressive drugs in this patient population decreases the risk of the patient’s visual acuity (VA) dropping below the 20/50 thresholds.
The study was performed by Anthony C. Gregory II, MD, MPH, and Jennifer E. Thorne, MD, PhD, at Johns Hopkins University School of Medicine in Baltimore, who worked with the Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study Research Group to examine a large retrospective cohort of patients with JIA-associated uveitis. The study included 327 children from five tertiary-care uveitis clinics. The children were relatively young at the age of JIA diagnosis (median age=4.1 years; range, 4 months to 16.9 years).
Finding Connections
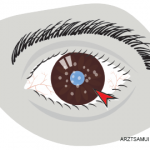
The investigators measured inflammation and vision loss. Specifically, they identified the presence of posterior synechiae, active anterior chamber inflammation, previous intraocular surgery, and vision loss across two VA thresholds (≤20/50 and ≤20/200). They found that posterior synechiae, active uveitis, and prior intraocular surgery were all statistically significantly associated with both VA thresholds at presentation and during follow-up.
Previously, studies have shown that the use of immunosuppressive drugs is associated with a reduced risk of at least moderate visual loss. The current study confirmed these results. The authors also found that the eyes of patients who had not developed ocular complications before presentation to the ophthalmology clinics were significantly less likely to develop ocular complications during follow-up visits.
Most eyes, however, were affected at presentation: 40.3% had a VA of ≤20/50, 24.2% had a VA of ≤20/200, and 60.2% had at least one ocular complication. The incidence of VA loss to the ≤20/50 threshold was 0.18 per eye-year (EY) and 0.09 per EY to the ≤20/200 threshold. The investigators calculated the incidence of developing at least one new ocular complication over follow-up as 0.15/EY.
Patients who had uveitis but whose eyes did not have complications at presentation had a 0.04/EY rate of developing at least one ocular complication during follow-up.
Increasing anterior chamber cell grade was associated with a dose-dependent increase in visual loss. In particular, active uveitis was associated with loss of VA for anterior chamber cell levels of 1+ or higher. Although the reduction in VA may be reversible in some cases, the authors assumed, when calculating risk of vision loss from uveitis, that the eyes never recover VA.
The authors acknowledge that their study may have had selection bias because patients who are more reliable and compliant with treatment and follow-up are more likely to receive immunosuppressive drugs. Nonetheless, the message to rheumatologists is clear. As Dr. Thorne told The Rheumatologist via e-mail, “Timely referral to a uveitis specialist appears to results in better visual outcomes, and use of immunosuppressive drugs (predominantly methotrexate) conferred a reduced risk of moderate visual loss. Further studies investigating the emerging role of biologics will be important to better understand their role in preventing visual loss.”
Egla C. Rabinovich, MD, MPH, co-chief of the division of pediatric rheumatology at Duke University School of Medicine in Durham, N. C., was not involved with the research, but reviewed the study to discuss it with The Rheumatologist. She emphasizes that uveitis is a serious disease that results in scarring in the eye and vision loss. She explains, “Some doctors and families have trouble getting their minds around the fact that this is a chronic disease. We shouldn’t be afraid of using immunomodulatory therapies in children to treat their uveitis.”
Dr. Pullen is a medical writer based in the Chicago area.
Reference