The American Medical Association’s (AMA) RVS Update Committee (RUC) and the Current Procedural Terminology Committee (CPT) meet six times per year to review resource costs and code descriptors for provider services. At these meetings, the ACR is represented by several volunteers and staff to provide a voice in shaping Medicare policy for rheumatology. The first half of 2018 has been packed with work for the ACR advisors and staff at both the RUC and CPT.
RUC Meeting Highlights
At the January 2018 AMA RUC meeting in San Diego, the ACR, along with the American College of Radiology, the Society of Nuclear Medicine and Molecular Imaging and the American College of Nuclear Medicine convened a consensus panel to present the practice expense data for dual-energy X-ray absorptiometry DXA for CPT code 77081. A compelling argument was made on two fronts to request an increase for clinical staff time, total cost of supplies and/or total cost of equipment. First, in the non-facility setting, the dominant provider was previously radiology, but it is now internal medicine. Second, there has been a change in the type of equipment typically used to perform this procedure. Current technology uses general-purpose fan beam units with accompanying computer and software. These units allow for highly accurate and repeatable DXA scanning at extremely low radiation doses.
It was also necessary to present more granular details regarding clinical staff time during the intra-service period when patients are properly positioned on the scan table to obtain an initial scan of the region of interest. The technologist confirms the adequacy of the image (e.g., proper positioning, adequate exposure, etc.). Positioning is compared with any prior study to ensure the patient was similarly positioned, and repeat imaging is performed if needed. The technologist defines the proximal and distal regions for analysis, ensuring that any metal, healed fractures, etc. are excluded. Images and bone mineral density data in report form are prepared for transmission to the picture archiving and communication system for reporting. The survey results and comparison with applicable codes support the recommended value for 77081, which was accepted by the AMA practice expense committee.
Additionally, the ACR RUC advisors are monitoring the work of the RUC’s Research Subcommittee, which is reviewing the existing pre- and postservice time packages, and will recommended new and revised time packages, if deemed necessary.
One key topic being monitored is the committee’s outline on how to define a complex patient, because this will affect whether the current packages need to be updated, as well as how to create non-facility postservice time packages. The work group is reviewing the packages, which include an analysis with the 25th percentile, median and 75th percentile pre- and postservice times, a comparison between the survey times and the final RUC recommendations for past packages with assigned times.
CPT Meeting Highlights
During the May 2018 CPT meeting in San Antonio, the CPT Editorial Panel received a code change application (CCA) from Anthem that requested a revision of the arthrocentesis code set (20600–20611) to include the phrase “image guidance,” because the current codes are specific to “ultrasound (US) guidance.” Anthem states that the combination services (bundling of injection/US) are narrow, and replacing “US” with “image guidance” will broaden the reach of the current code set.
As one of the original societies involved in revising the code set, the ACR stated it did not support the request; the current CPT codes for arthrocentesis code series 20600–20611 already allow specificity and clarity for the code set. Thus, the change could allow unnecessary overutilization of other imaging equipment and dilute the value of the code descriptor. The code change is, therefore, needless. The level of work and equipment in the existing code set is typical; the work, cost and complexity are different and should remain separately reportable. For example, fluoroscopy or CT-guided imaging both present radiation exposure, requiring the study room to have adequate shielding, and there are different regulation requirements to be met than with US. US image interpretation is distinct and fundamentally different than looking at a conventional radiograph/fluoroscopy. Also, the parenthetical included in the code sets clearly defines how to appropriate code for other modalities in the 70000 series, which is consistent with coding guidelines for the intended use of the code(s).
Further, changing the code descriptor to “image guidance” would be beyond the RUC mandate and create additional RUC ramifications. This change would not be editorial, but would require a new code change application and resurveying, which will be difficult given the infrequent use of the other types of imaging guidance for these procedures. Fluoroscopic guidance and US guidance have significantly different practice expenses associated with them, and the current codes are valued with US guidance bundled. The CPT Editorial Panel voted not to accept the code change request from Anthem.
The Importance of Input
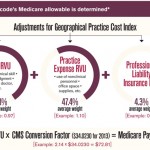
The work at the AMA RUC and CPT meetings is filled with regular reviews of procedures and services to determine whether they are appropriately valued or overvalued for the Medicare physician fee schedule. It is crucial the ACR participate in these meetings because it allows the College to provide input about the medical services performed by rheumatology providers, who are on the front lines of caring for patients every day.
The ACR representatives to the AMA RUC committee include Timothy Laing, MD, Eileen Moynihan, MD, Deborah Desir, MD and Fredrica Smith, MD. For the AMA CPT Editorial Committee, the ACR representatives include Dr. Laing and Joseph Huffstutter, MD.
For questions or additional information on RVUs or the CPT coding process, contact ACR staff liaison Antanya Chung.