Bortezomib, a proteasome inhibitor developed for use in myeloma treatment, has produced responses in many patients with immunoglobulin light chain amyloidosis (AL), so survival from diagnosis can now range from eight to 10 years in many patients. However, Dr. Pepys also said roughly one-quarter of all patients with AL amyloidosis still die within six months of diagnosis. The monoclonal antibody developed for myeloma, daratumumab, also targets the plasma cells that cause AL amyloidosis and, therefore, holds much promise for treating this condition.
But major treatment challenges remain. Although AL patients with low-risk disease can do well if treated aggressively with full-dose chemotherapy, those with intermediate risk might not tolerate full-dose treatment, and their responses can suffer. And those with high-risk disease are even less tolerant of aggressive treatment and have even worse outcomes.
In his research, Dr. Pepys has focused on serum amyloid P component (SAP), a normal blood protein present in everybody, and has used it in both imaging and treatment. SAP is produced in the liver and secreted into the blood, and as it circulates around, it sticks to amyloid if it’s present. When it sticks, there’s much more of it in the amyloid than in the blood—a feature Dr. Pepys called a “dynamic equilibrium.”
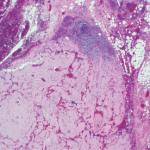
By radiolabeling SAP and injecting it into the circulation, clinicians can visualize this equilibrium by imaging amyloid deposits throughout the body. This provides extensive and valuable information not available just from tissue biopsy.
At the UK’s National Amyloidosis Center and elsewhere, researchers began gathering evidence that SAP was not just there by happenstance—it actually contributed to the pathogenesis of amyloidosis, stabilizing the fibrils when it binds to them and even promoting amyloid formation.
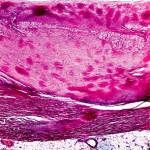
After SAP knockout mice were found to take longer to develop amyloid deposition and develop less of it, Dr. Pepys, in collaboration with Roche, created a small molecule to remove SAP from amyloid, on the theory that “if you removed all the SAP from the amyloid, the body would recognize the abnormal fibrils, and macrophages would come along and get rid of them.” Unexpectedly, the drug they produced, miridesap, removed SAP and reduced the amount of SAP in the amyloid deposits. But it did not remove all of it from the deposits, so the amyloid persisted.
Dr. Pepys then realized that after clearing SAP from the blood with miridesap, it would become possible to treat patients with antibodies directed against SAP. The antibodies could home on SAP as a specific marker for amyloid and, once there, trigger the body’s normal, highly effective mechanism for removing abnormal debris from tissue.