cyclosporin A, that have been altered to be non-immunosuppressive. These derivatives are known to inhibit the leukocyte attracting function of cyclophilins. Dr. Constant hopes to learn whether they reduce joint inflammation and to gain insights into the mechanisms involved.
At the June meeting, Dr. Constant presented data comparing changes in different inflammatory markers after treatment with the two analogs, using mouse models of inflammation. One of the analogs penetrates cells and therefore targets both intracellular and extracellular sources of cyclophilins; the second has been modified to work only on extracellular cyclophilins. “So there will be no accumulation of the drug inside the cells,” she said.
In mice with allergic asthma, the analog targeting only extracellular cyclophilins produced a greater reduction in a variety of inflammatory markers, she said. The next step is to test this analog, which Dr. Constant has “high hopes for,” in collagen-induced arthritis in mice. That study will be conducted within the next year, she said.
The parent drug involved, cyclosporin A, has already been well studied in patients, she said. “We believe it will have fewer side effects because it will not have any impact on intracellular cell function, like signaling, and so it will only target cellular events that are regulated outside the cell.”
Inhibiting PAD Activity
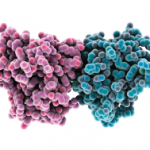
Paul R. Thompson, PhD, presented the work that his research team has been pursuing—first at the University of South Carolina in Columbia and more recently at Scripps Florida in Jupiter, Fla.—to decipher the role that protein arginine deiminases (PADs), and specifically PAD4, plays in the development of RA. Increased PAD4 activity has been identified in RA and dysregulated activity of the enzyme family has been associated with a number of other diseases, including cancer, multiple sclerosis, and ulcerative colitis.
Dr. Thompson’s ongoing research, conducted with collabortors at the University of Colorado, has been looking at whether specific compounds can inhibit PAD4 activity as a strategy to treat RA. At the meeting, he presented findings on disease incidence and severity in mouse models following injections with one of two PAD inhibitors, Cl-amidine and F-amidine.
In these experiments, the mice were immunized with type II collagen (CII) in complete Freund’s adjuvant (CFA) and boosted at Day 15 in induce collagen-induced arthritis. Then they were monitored for at least 40 more days. The disease severity was lower in the group that received daily injections of Cl-amidine compared with F-amidine.
In a subsequent study, the mice received the CII/CFA immunization initially, were boosted at 21 days, and then were tracked for at least 14 more. Meanwhile, the effectiveness of Cl-amidine treatment was assessed at various dose levels. In a dose-dependent way, the compound decreased the disease severity by as much as 55% percent, said Dr. Thompson, a biochemist and associate professor in the Department of Chemistry at Scripps Florida.