ACR CONVERGENCE 2021—Pulmonary disease is a potentially serious, yet oft-underdiagnosed complication of Sjögren’s syndrome. Fortunately, Consensus Guidelines for the Evaluation and Management of Pulmonary Disease in Sjögren’s were released in 2021.1 The guidelines were initiated and supported by the Sjögren’s Foundation. Pulmonologists, rheumatologists and patients worked together to finalize the document.
ACR CONVERGENCE 2021—Pulmonary disease is a potentially serious, yet oft-underdiagnosed complication of Sjögren’s syndrome. Fortunately, Consensus Guidelines for the Evaluation and Management of Pulmonary Disease in Sjögren’s were released in 2021.1 The guidelines were initiated and supported by the Sjögren’s Foundation. Pulmonologists, rheumatologists and patients worked together to finalize the document.
During ACR Convergence 2021, a pulmonologist and a rheumatologist, both of whom helped craft the guidelines, discussed the diagnosis and management of pulmonary manifestations of Sjögren’s syndrome.
Pulmonary Manifestations of Sjögren’s Syndrome
Approximately one in six patients living with Sjögren’s syndrome has pulmonary involvement, which is associated with higher mortality and lower quality of life compared with patients with Sjogren’s syndrome who do not have pulmonary involvement. Augustine S. Lee, MD, MSc, FCCP, chair of the Division of Pulmonary Medicine, Mayo Clinic Florida, Jacksonville, reviewed common pulmonary manifestations in Sjögren’s syndrome and the recommended approach.
1. Sjögren’s syndrome with no respiratory symptoms
“Screening for pulmonary disease is of utmost importance [because] 10–20% of patients [with Sjögren’s syndrome] will have clinically relevant pulmonary involvement,” Dr. Lee said.
Screening should include a careful respiratory history, cardiopulmonary exam, a baseline chest radiograph and baseline complete pulmonary function testing (PFT; i.e., spirometry, lung volumes, diffusing capacity of the lungs for carbon monoxide [DLCO]), and resting and exercise oxygen saturation readings.
2. Sjögren’s syndrome with a cough
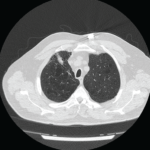
In a patient with Sjögren’s syndrome who has pulmonary symptoms, the recommendation is to obtain high-resolution computed tomography (CT) of the chest—as opposed to a chest radiograph—in addition to complete PFTs.
“[A chest radiograph] may miss 10–15% of significant disorders, such as interstitial lung disease [ILD], neoplasms or bronchiolar diseases,” Dr. Lee said. “Of note, the [high-resolution CT] should include expiratory views. This is particularly important because of the potential for small airway involvement in Sjögren’s syndrome, which standard inspiratory views on the [high-resolution CT] and PFTs will not detect. Prone imaging should also be considered if needed to differentiate dependent subpleural atelectasis from ILD.”2
Dr. Lee continued, “Although evaluation for more nefarious etiologies is paramount, the most likely cause of cough in Sjögren’s syndrome remains xerotrachea. Common associations, such as gastroesophageal reflux disorder, asthma and rhinitis, should also be considered.”
3. Sjögren’s syndrome with ILD
About 25% of patients with Sjögren’s syndrome will have ILD, with nonspecific interstitial pneumonia (NSIP) being the most common subtype (45%). Fortunately, lung biopsy is typically not required for diagnosis, and treatment is based on the pattern of ILD, symptoms, degree of lung dysfunction and clinical course.3
“The guidelines provide flow-diagramed specifics,” said Dr. Lee, “but in general, patients should be monitored with PFTs and pulse oximetry. Supportive measures, such as oxygen and pulmonary rehabilitation, are important parts of therapy. I consider adding anti-fibrotics to patients with clear fibrotic patterns [e.g., usual interstitial pneumonia] or after failing or progressing despite standard anti-inflammatory therapies. Transplant should be entertained early in patients who are rapidly deteriorating or in patients with significant oxygen requirements.”
4. Sjögren’s syndrome with nodules
“It’s important to remember that about 50% of the population will have lung nodules based on CT screening,” Dr Lee said. “If found, these nodules should be monitored according to Fleischner Society Guidelines to monitor for lung cancer. In Sjögren’s syndrome, lung nodules may represent pulmonary lymphoma, and positron emission tomography [PET] can be helpful in this situation if the lesion is approaching a centimeter in size. Prior to an invasive biopsy, I recommend talking to your friendly neighborhood oncologist.”4,5
5. Sjögren’s syndrome with pulmonary consolidation
Ten to 35% of pulmonary consolidation in Sjögren’s is caused by infectious pneumonia, especially given increased risk with immunosuppressants and loss of the normal mucociliary barrier. “However, other etiologies, such as organizing pneumonia and pulmonary lymphoma, should be considered if [the patient] does not improve or respond to empiric treatment [of their pneumonia]. The best test in most of these situations [i.e., patients with consolidation] is bronchoscopy,” Dr. Lee said.
In summary, pulmonary manifestations in Sjögren’s syndrome are common and variable. Some manifestations are asymptomatic, but some can have severe complications (e.g., ILD and lymphoma). Thus, vigilance is necessary. Biopsy is needed where neoplasm is a concern, although not typically required for evaluation of ILD or airway diseases.
“Overall, I recommend careful clinical screening of all patients [with Sjögren’s syndrome], including a baseline [chest radiograph] and complete PFTs. If the patient is symptomatic or has an abnormal PFT or [chest radiograph], a [high-resolution CT] with expiratory views should be considered,” Dr. Lee concluded.
Multidisciplinary Teamwork
Nancy Carteron, MD, FACR, clinical professor of medicine, Division of Rheumatology, University of California, San Francisco, health sciences clinical professor, Sjögren’s Clinic, Herbert Wertheim School of Optometry & Vision Science at the University of California, Berkeley, and rheumatology chair, Sjögren’s Foundation Clinical Practice Guidelines, addressed the multidisciplinary assessment and management of pulmonary manifestations in patients with Sjögren’s syndrome.
Dr. Carteron reinforced that lung involvement in Sjögren’s syndrome is common and under-recognized. She stressed the importance of early detection of pulmonary disease to optimize the care of our patients, especially because the diagnosis of Sjögren’s syndrome is often delayed.6 She championed a multi-disciplinary approach for the diagnosis and management of patients with Sjögren’s syndrome and pulmonary involvement.
“Collaboration improves diagnosis and decreases time to a consensus treatment plan. Disease knowledge can be shared across specialties, and the patient hopefully can see several specialists on the same day,” she said.
To conclude the session, Dr. Carteron drew the audience’s attention to cystic lung disease in Sjögren’s syndrome, a complication of which she was not particularly aware prior to working on the new consensus guidelines herself.
“Cystic lung disease appears to be more common in [Sjögren’s syndrome] than other connective tissue diseases,” she explained. “It’s associated with lymphocytic interstitial pneumonia [LIP] and lymphoid follicular bronchiolitis, and may suggest the presence of amyloid or mucosa-associated lymphoid tissue [MALT] lymphoma, especially if associated with nodules. Furthermore, cysts may become infected or rupture, leading to pneumothorax. There is more we have to learn about this entity, but we should all keep this in mind when caring for patients [with Sjögren’s syndrome].”7–9
Summary
Pulmonary disease is common, variable and frequently underdiagnosed in Sjögren’s syndrome. New consensus guidelines provide much needed guidance to our community regarding screening, monitoring and management of these patients. Close collaboration with our pulmonary colleagues, as well as other specialists, optimizes care.
Samantha C. Shapiro, MD, is an academic rheumatologist and an affiliate faculty member of the Dell Medical School at the University of Texas at Austin. She received her training in internal medicine and rheumatology at Johns Hopkins University, Baltimore. She is also a member of the ACR Insurance Subcommittee.
References
- Lee AS, Scofield RH, Hammitt KM, et al. Consensus guidelines for evaluation and management of pulmonary disease in Sjögren’s. Chest. 2021 Feb;159(2):683–698.
- Franquet T, Díaz C, Domingo P, et al. Air trapping in primary Sjögren syndrome: Correlation of expiratory CT with pulmonary function tests. J Comput Assist Tomogr. Mar–Apr 1999;23(2):169–173.
- Flament T, Bigot A, Chaigne B, et al. Pulmonary manifestations of Sjögren’s syndrome. Eur Respir Rev. 2016 Jun;25(140):110–123.
- Casal Moura M, Navin PJ, Johnson GB, et al. Pulmonary nodules in patients with primary Sjögren’s syndrome: Causes, clinico-radiologic features and outcomes. Respir Med. Nov–Dec 2020;174:106200.
- MacMahon H, Naidich DP, Goo JM, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: From the Fleischner Society 2017. Radiology. 2017 Jul;284(1):228–243.
- Huang YT, Lu TH, Chou PL, et al. Diagnostic delay in patients with primary Sjögren’s syndrome: A population-based cohort study in Taiwan. Healthcare (Basel). 2021 Mar 23;9(3):363.
- Lechtman S, Debray MP, Crestani B, et al. Cystic lung disease in Sjögren’s syndrome: An observational study. Joint Bone Spine. 2017 May;84(3):317–321.
- Martínez-Balzano CD, Touray S, Kopec S. Cystic lung disease among patients with Sjögren syndrome: Frequency, natural history and associated risk factors. Chest. 2016 Sep;150(3):631–639.
- Baqir M, Kluka EM, Aubry MC, et al. Amyloid-associated cystic lung disease in primary Sjögren’s syndrome. Respir Med. 2013 Apr;107(4):616–621.