Patients with diffuse systemic sclerosis (dSS) with an associated ANCA-positive vasculitis have been infrequently described. In this article, we report the case of a 53-year-old woman, previously diagnosed with dSS, who developed an ANCA-associated vasculitis, which manifest as peripheral nerve and muscle disease.
Scleroderma is a disease characterized by sclerosis of the skin and visceral organs, vasculopathy, Raynaud’s phenomenon and the presence of autoantibodies. The disease spectrum is wide, with systemic and localized forms, depending on the extent of skin thickening. There is also a vasculopathy involving multiple organ systems that leads to the presence of cutaneous and mucosal telangiectasias, digital ulcers and tissue ischemia. Medium-size vessels can also be involved, sometimes leading to scleroderma renal crisis or pulmonary artery hypertension. However, scleroderma is rarely associated with an ANCA-positive vasculitis. We report this unique situation.
Case Report
A 53-year-old woman was admitted to our hospital with weakness and numbness in her legs. She had been diagnosed with Raynaud’s phenomenon 10 years before, followed by the development of autoimmune hypothyroidism. Three years later, she complained of telangiectasias spreading over her face and neck, and she developed a digital ulcer on her middle finger. She noted a dry cough and dyspnea on exertion. The ANA and the anti-topoisomerase antibodies (Scl-70) were positive. She was diagnosed with dSS with pulmonary involvement (moderate to severe pulmonary fibrosis).
There was no evidence for pulmonary hypertension, or cardiac or esophageal involvement. After being treated for a presumed episode of pneumonia, she failed to significantly improve, and her cough and dyspnea worsened. She complained of weakness and numbness in her distal lower extremities with preserved muscle strength and hypoesthesia to touch.
The development of vasculitis in patients with systemic sclerosis is highly uncommon.
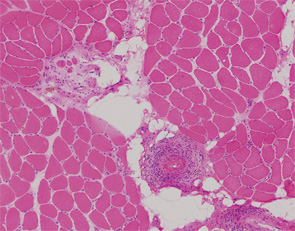
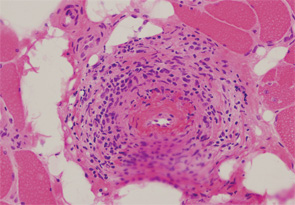
Initial laboratory tests included a normocytic and normochromic anemia, thrombocytosis, elevated acute-phase reactants and normal serum creatinine. MPO-ANCA titer was 174 AU (normal <10 UI/mL). PR-3-ANCA was negative. Antiglomerular basal membrane and anti-Jo-1 antibodies were negative, and complement C3 and C4 were within normal limits. An electromyogram showed evidence of a moderate myopathy without polyneuropathy or myositis. A muscle and peripheral nerve biopsy demonstrated features of a necrotizing vasculitis with signs of axonal degeneration and severe denervation attributable to ischemic neuropathy (see figures, right).
Therapy was initiated with a high dose of prednisolone (bolus of 1 mg/kg/day IV for three days, followed by 60 mg PO daily) and cyclophosphamide treatment (five monthly IV boluses of 750 mg each) was initiated. A few weeks later, maintenance immunosuppressive therapy was introduced with azathioprine (150 mg day PO), and her hypoesthesia and weakness gradually disappeared.



