SNOWMASS VILLAGE, COLO.—The study of anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) is ongoing, and research results should help improve treatment for this patient population. Key trials and therapeutic options were discussed at the 2020 ACR Winter Symposium during the session, Update on the Treatment of ANCA-Associated Vasculitis, by Peter A. Merkel, MD, MPH, chief of the Division of Rheumatology, director of the Penn Vasculitis Center, and professor of medicine and epidemiology at the University of Pennsylvania.
“This past year has seen the release of the results of several major trials that will change the standard of care for patients with [AAV],” Dr. Merkel said. “These new data will be of great interest and relevance to practicing rheumatologists.”
Standard of Care
AAV is a group of diseases characterized by the destruction and inflammation of small- and medium-caliber vessels and includes microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA) and eosinophilic granulomatosis with polyangiitis.
Although treatment for AAV has advanced substantially in the past few decades, there are still many unmet needs. In particular, less toxic regimens, more rapid induction of remission and prevention of relapse remain important research goals.
Current therapy for non-severe disease includes combining glucocorticoids with methotrexate or rituximab. For more severe disease, therapy options include:
- Combining glucocorticoids with rituximab or cyclophosphamide, followed by maintenance of remission with any of several agents, including rituximab, azathioprine or methotrexate;
- Plasma exchange, which has been highly controversial; and
- Novel agents, especially inhibitors of C5a, trials of which have been highly encouraging.
Key Multi-Center Trials
The 2014 MAINRITSAN study was an open-label, randomized, controlled trial that included 115 patients with AAV who attained remission after treatment with cyclophosphamide and glucocorticoids.1 Patients were randomized to receive rituximab (500 mg intravenously) or azathioprine (which was tapered at one year). Results showed more patients had sustained remission at 28 months with rituximab than azathioprine.
After this study, several questions remained to be investigated, Dr. Merkel said. Key among them: What about patients who didn’t receive cyclophosphamide for induction? Will lower-dose glucocorticoids work as well? What predicts relapse or sustained remission?
After MAINRITSAN, studies have looked into some of these and other questions to help elucidate the therapeutic potential of existing and emerging treatments.
RITAZAREM was an open-label, randomized, controlled trial that compared rituximab with azathioprine as a maintenance therapy in relapsing AAV for 190 patients with GPA/MPA who were enrolled during a relapse of their vasculitis and treated with rituximab.2 At four months, 170 patients attained remission and then were randomized to different treatment groups: 85 patients received maintenance treatment with 1,000 mg of rituximab every four months, and 85 received azathioprine 2 mg/kg/day. In addition, patients’ glucocorticoid doses were tapered. Treatment ended at month 24 with follow-up out to 36–48 months.
Initial results of RITAZAREM, presented at a plenary session at the 2019 ACR/ARP Annual Meeting, showed that rituximab was superior to azathioprine for preventing disease relapse in AAV patients with a prior history of relapse.3 The study didn’t uncover any new major safety signals for use of these medications in this population either, said Dr. Merkel, one of the two principal investigators of the international trial.
“The results of the MAINRITSAN and RITAZAREM [trials] firmly establish the role of rituximab in maintenance of remission in AAV,” Dr. Merkel said.
Plasma Exchange
Plasma exchange has been used in addition to glucocorticoids and immunosuppressive agents, with mixed results, to treat patients with AAV. A retrospective, single-center series found no benefit for alveolar hemorrhage or glomerulonephritis, and a meta-analysis in the April 2011 issue of the American Journal of Kidney Diseases was inconclusive, Dr. Merkel said.4
“Controversy and clinical equipoise existed,” he added. “This led us to design and conduct the PEXIVAS trial.”
PEXIVAS was a two-by-two factorial, randomized, investigator-initiated trial that included 704 patients randomized in centers across Europe, North America, Asia and Australasia to receive plasma exchange or no plasma exchange; the second aspect of the trial compared the use of the usual schedule of high-dose glucocorticoids compared with a schedule that prescribed approximately half as much glucocorticoids. All patients also received immunosuppression with either cyclophosphamide or rituximab.
An article by Dr. Merkel and colleagues published in the Feb. 13, 2020, issue of the New England Journal of Medicine reported the results of the PEXIVAS trial.5 Plasma exchange did not reduce the composite of mortality or end-stage renal disease, but the reduced-dose schedule of glucocorticoids was non-inferior to a “standard” dose and resulted in fewer serious infections.
“The results of PEXIVAS do not support the routine use of plasma exchange for induction of remission for patients with severe AAV, [but] do support the use of a reduced-dose schedule for glucocorticoids,” Dr. Merkel said. “These results will change the standard of care for patients with severe AAV.”
Novel Agents
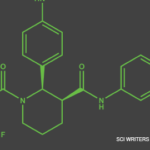
Avacopan, formerly known as CCX168, is a novel, oral, small-molecule drug that is a selective inhibitor of the component C5a receptor (C5aR). A phase 2 trial published in 2017 the Journal of the American Society of Nephrology concluded that C5aR inhibition with avacopan was effective as a replacement for high-dose glucocorticoids in treating vasculitis.6
Avacopan was investigated further in ADVOCATE, an industry-sponsored phase 3 trial that involved 331 patients with active AAV who were all given either rituximab or cyclophosphamide, and randomized to receive avacopan with no glucocorticoids after the first few weeks or placebo and usual-dose glucocorticoids. Dr. Merkel shared the top-line results of the trial, which demonstrated that adding avacopan to either rituximab or cyclophosphamide allows for treatment of AAV with a minimized glucocorticoid regimen.7
Results showed disease remission at 26 weeks and sustained remission at 52 weeks compared with the standard of care, and patients taking avacopan had reduced glucocorticoid-related toxicity and significant improvements in quality of life and in renal function. The full results of the ADVOCATE study are expected to be published later this year by Dr. Merkel and colleagues.
Evolving Treatments
The results of RITAZAREM, PEXIVAS and ADVOCATE are expected to have a major impact on the approach physicians and patients take to the treatment of AAV.
“Studying the comparative effectiveness of varying glucocorticoid dosing schedules and steroid-sparing regimens in AAV is challenging but can be done and is being done,” Dr. Merkel said. “Ongoing and planned trials in AAV will continue to lead toward safer and more effective therapies for this form of vasculitis and provide increasing benefit to patients.”
Kimberly Retzlaff is a freelance medical journalist based in Denver.
References
- Guillevin L, Pagnoux C, Karras A, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014 Nov 6;371(19):
1771–1180. - Barnard C. Support for rituximab maintenance therapy in ANCA-associated vasculitis. medwireNews. 2019 Nov 10.
- Smith R, Jayne D, Merkel P. A randomized, controlled trial of rituximab versus azathioprine after induction of remission with rituximab for patients with ANCA-associated vasculitis and relapsing disease [abstract]. Arthritis Rheumatol. 2019;71(suppl 10).
- Walsh M, Catapano F, Szpirt W, et al. Plasma exchange for renal vasculitis and idiopathic rapidly progressive glomerulonephritis: A meta-analysis. Am J Kidney Dis. 2011 Apr;57(4):566–574.
- Walsh M, Merkel PA, Peh C-A, et al. Plasma exchange and glucocorticoids in severe ANCA-associated vasculitis. N Engl J Med. 2020 Feb 13;382(7):622–631.
- Jayne DRW, Bruchfeld AN, Harper L, et al. Randomized trial of C5a receptor inhibitor avacopan in ANCA-associated vasculitis. J Am Soc Nephrol. 2017 Sep;28(9):2756–2767.
- ChemoCentryx and VFMCRP announce positive topline data from pivotal phase III ADVOCATE Trial demonstrating avacopan’s superiority over standard of care in ANCA-associated vasculitis (press release). 2019 Nov 25.