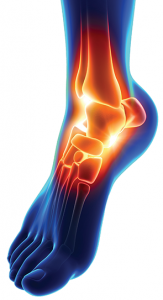
Four ankle prostheses are approved for use in the U.S. They do not require the bones to be fused.
Image Credit: decade3d – anatomy online/shutterstock.com
Ankle arthritis is a debilitating condition that leaves many patients in severe pain and greatly limits their activities. Until recently, the standard treatment for bone-on-bone ankle pain has been ankle fusion, or arthrodesis, in which surgeons literally fuse the bones of the ankle joint together. However, in the past few years, total ankle replacement surgery, also known as total ankle arthroplasty (TAA), has emerged as an alternate treatment for those with end-stage arthritis of the ankle.
History of Ankle Replacements
According to a Wall Street Journal article from November 2014, 26% of all ankle surgeries were replacements in 2010, up from 13% in 2007, and the global market for total replacement has grown 15% to 20% annually for the last several years, with 16,000 procedures completed in 2014.1
The first generation of devices used for ankle replacement in the mid-1970s yielded mixed results, but in the late 1990s, newer implants were developed that boast a higher success rate. Today, four ankle prostheses are approved for use in the U.S. These new designs don’t require the bones to be fused; instead, bone grows into the ankle prosthesis similar to hip and knee replacements.
Although fusions do alleviate pain in patients, the procedure also limits range of motion and mobility. In contrast, TAA is designed to mimic the natural movements of the ankle, allowing patients to safely resume light recreational activities and non-weight-bearing sports after surgery.
In addition, fusion also increases the chance of developing arthritis in adjacent bones due to ankle immobility, whereas TAA takes stress off the joints below and in front of the ankle, decreasing the risk of arthritis developing there.
Despite the growing popularity and benefits of TAA, many doctors and patients still aren’t aware that ankle joints can be successfully replaced.
Candidates
“Patients often tell us they didn’t realize TAA was an option for them,” says Dr. Shannon Rush, DPM, FACFAS, a Fellow of the American College of Foot and Ankle Surgeons and a surgeon at Palo Alto Medical Foundation in Mountain View, Calif. “I encourage rheumatologists who have patients that suffer from debilitating ankle pain to consider having them evaluated as candidates for TAA, especially before prescribing opioids.”
Dr. Rush says patients who don’t find relief through bracing or medications should be referred to a surgeon who is experienced in ankle replacement surgery for evaluation. Good candidates for TAA include those who have a joint that has been severely damaged by injury, osteoarthritis or rheumatoid arthritis. Patients who have had a prior ankle surgery, such as ankle fusion surgery, are also candidates for TAA.
Unlike hip and knee surgery traditionally performed on seniors, the majority of TAA patients are younger.
“I’ve had patients with RA who have been in their late 30s and undergone ankle replacement,” Dr. Rush says. “Most patients who undergo TAA are in their 40s and older.”
Contraindications
Dr. Rush says patients with poor circulation (peripheral artery disease) or loss of sensation (neuropathy), or those who have a significant deformity related to a birth defect or previous traumatic event, are not good candidates for ankle replacement surgery.
In addition, elderly or sedentary patients, those who are overweight or those who have comorbidities are considered better candidates for ankle fusion.
Helping Patients Regain Their Quality of Life
Mary Davis, 67, of Salem, Ore., says her ankle woes started when she was a high school basketball player. Ten years later, Ms. Davis tore the ligaments in her ankle and underwent surgery to repair the damage.
Over the years, Ms. Davis’ ankle continued to deteriorate. Although she taped it each morning, over time her ankle became swollen and painful, and it limited her ability to participate in the wide range of sports that she enjoyed.
In summer 2013, Ms. Davis made an appointment to see Kelly McCormick, MD, an orthopedic surgeon with Hope Orthopedics in Salem, Ore.
“After an evaluation, Dr. McCormick said I was a good candidate for either fusion or ankle replacement surgery,” Ms. Davis says. “He explained TAA devices have gotten better than ever, and that implants are expected to last longer than 10 years.”
Ms. Davis first considered ankle fusion, but after Dr. McCormick suggested she try wearing a walking boot that would simulate how her ankle would feel after surgery, she opted to undergo TAA instead.
“With ankle fusion, I found that I [would lose] range of motion,” Ms. Davis says. “I wanted to walk with a normal gait, to play with my grandchildren and to participate in sports and other activities that I couldn’t do comfortably with a fusion.”
In October 2013, Ms. Davis underwent TAA surgery, performed by Dr. McCormick, in a procedure that took approximately two hours.
After making an incision on the side of the ankle, Dr. McCormick removed the arthritic bone and cartilage from Ms. Davis’ tibia and talus. Dr. McCormick then inserted the implant, consisting of two metal components and a plastic spacer, to form a new ankle joint.
“I think TAA is one of the most satisfying surgical procedures,” Dr. McCormick says. “When patients first come to me, they are in so much pain and are so limited in what they are able to accomplish on a daily basis. It’s liberating to see these same patients resume an active, pain-free life after surgery.”
Although every surgeon has different criteria, Dr. McCormick says he prefers to perform TAA on patients who are 55 or older and who have low to moderate activity levels.
“With younger patients, there is a greater risk of wearing out the ankle prosthesis quicker,” Dr. McCormick says. “Someone who is young and runs marathons would be a better candidate for ankle fusion.”
After an overnight stay in the hospital, Ms. Davis went home to begin her recovery, a process that lasts six weeks for most TAA patients.
“Within 10 days after my surgery, I was pain free,” says Ms. Davis, who used a cane to avoid putting weight on her ankle. She attended regular physical therapy sessions and by March, Ms. Davis had resumed playing sports, including tennis.
“I couldn’t have asked for better results,” Ms. Davis says. “I spent two years not being able to wear cute shoes because I was in such debilitating pain. One of the first things that I did when I was able to walk unassisted after surgery was to go shoe shopping.”
The Future of Ankle Replacement Surgery
Although it doesn’t have the same long-term track record as hip or knee replacement surgery, Dr. Rush says shorter-term studies on the newer devices used for ankle replacement surgery are very promising, with the newer generation of implants anticipated to last 10–15 years.
This past May, the Hospital for Special Surgery (HSS) in New York announced it had received a grant from the American Orthopedic Foot and Ankle Society to compare the biomedical differences in function between patients who underwent TAA with those who received ankle fusion.2 Dr. Rush notes that other studies are being conducted to determine the lifespan of TAA implants.
“We know that while the plastic lining of the implant may wear out after several years, it can often be replaced without revising the metal components,” Dr. Rush says. “Ankle arthritis is one of the most debilitating health conditions, and one that affects all areas of a patient’s life. We’ve seen how TAA can offer patients the chance to live pain free and walk with ease again.”
Linda Childers is a health writer located in the San Francisco Bay Area of Northern California.
References
- Landro L. More patients opt to replace ankle joints instead of fusion: Increased range of motion; expect repeat surgery a decade later. The Wall Street Journal. 2014 Nov 24.
- Hospital for Special Surgery. Researchers at hospital for special surgery receive grant to study health outcomes of ankle fusion versus replacement.

