In this cohort, 50.2% of patients were found to have an axial spondyloarthritis and 17.5% of patients had a peripheral spondyloarthritis, based on Assessment of SpondyloArthritis International Society criteria; the prevalence of spondyloarthritis was even higher among HLA-B27-positive patients than HLA-B27-negative patients (69.8% vs. 27.3% with axial disease, 21.9% vs. 11.1% with peripheral disease, respectively). The authors noted that numerous patients with anterior uveitis are likely to have undiagnosed spondyloarthritis and should be screened for these conditions.
The prevalence of uveitis may be as high as 33% in patients with ankylosing spondylitis.
Similarly, researchers from Dublin, Ireland, recruited 104 consecutive patients with presumed idiopathic acute anterior uveitis who presented to the ophthalmology emergency department over the course of one year.5 These patients each underwent a standardized evaluation that included testing for HLA-B27; clinical screening for symptoms and signs of axial or peripheral arthritis or enthesitis; personal or family history of psoriasis, inflammatory bowel disease or other spondyloarthropathy; and radiographs of the sacroiliac joints and other joints as clinically indicated. Using this algorithm, 41.6% of the patients were found to have undiagnosed spondyloarthropathy, and this algorithm (termed the Dublin Uveitis Evaluation Tool) has now been validated as an instrument to assist first-line clinicians in recommending appropriate referral of uveitis patients to rheumatology clinics.
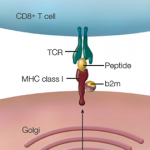
Screening for HLA-B27
In her own practice, Dr. Thorne makes sure to diligently screen for HLA-B27 status and for signs of conditions like ankylosing spondylitis, while also evaluating for diseases that include syphilis, tuberculosis, Lyme disease, sarcoidosis and other causes of uveitis. The one point Dr. Thorne stresses for rheumatologists: It is essential to counsel ankylosing spondylitis and other spondyloarthritis patients early and often that it’s critical to report any visual symptoms to allow for early ophthalmologic evaluation.
Any spondyloarthritis patient with a red and/or painful eye, new onset of blurry vision, sensation of flashing lights or floaters should be seen quickly by an ophthalmologist, who can perform a slit-lamp examination and evaluate for uveitis. Failure to arrange for this early evaluation can result in misdiagnosis and prolonged or recurrent symptoms for patients, causing them needless suffering.
Close Coordination of Care Necessary
First-line treatment for uveitis typically includes topical or injectable corticosteroids, but the severity of disease and frequency of recurrence will dictate if additional treatments are needed. These treatments may include oral corticosteroids, methotrexate, mycophenolate mofetil and, if necessary, the addition of biologic treatments, such as tumor necrosis factor inhibitors, anti-interleukin 6 agents, calcineurin inhibitors and B cell depleting agents, such as rituximab. Close coordination of care is needed between ophthalmologists and rheumatologists to effectively treat the disease, monitor for medication side effects and long-term adverse effects, and ensure patients feel supported with regard to all manifestations of their systemic disease.