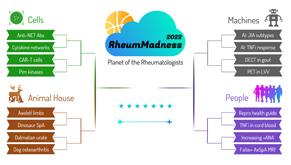
 Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The more your picks match those of our Blue Ribbon Panel of rheumatologists, the more points you get. Learn more about the panel and how the brackets work online.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn more on the RheumMadness website.
Region: Machines Team: DECT in Gout
Gout is such a pain in the toe. It’s one of the most common forms of inflammatory arthritis in adults, yet the diagnosis can be polarizing. The diagnosis of gout typically involves the detection of monosodium urate crystals in synovial fluid or other tissue samples. Despite being the diagnostic gold standard, this approach poses challenges, namely the unpredictability of synovial fluid specimen sampling (Did anyone say, “dry tap”?) and inaccurate recognition of crystals on polarized microscopy (*squints* Is that a crystal or glove dust?).
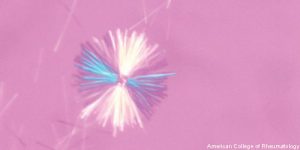 Due to the fundamental differences that exist between treating gouty arthritis and other types of inflammatory arthritis, the inability to precisely detect monosodium urate crystals may lead to needless, ineffectual and potentially harmful treatments.1,2
Due to the fundamental differences that exist between treating gouty arthritis and other types of inflammatory arthritis, the inability to precisely detect monosodium urate crystals may lead to needless, ineffectual and potentially harmful treatments.1,2
If you are like us—with a fist to the sky crying out, “There must be another way!”—you’ve come to the right place.
Repurposing of non-invasive imaging techniques, such as dual-energy computed tomography (DECT) and ultrasound, has led to consequential advances in the diagnosis of gout. To analyze the diagnostic accuracy of DECT, ultrasound or a combination of the two for gout of the feet and ankles and/or knees, a prospective study was performed over approximately three years with 147 patients at a single outpatient rheumatology clinic in a tertiary care hospital.
The patients were mainly middle-aged men with a mean duration of symptoms of 9.2 years. One-third of the patients underwent synovial fluid aspiration with 79% had monosodium urate crystals (gold standard). Two-thirds of the patients met the modified 2015 ACR EULAR gout classification (silver standard). The study investigated:
- Sensitivity;
- Specificity;
- Positive predictive value (PPV);
- Negative predictive value (NPV); and
- Overall accuracy of DECT and ultrasound both alone and in combination at various bony sites, as expressed by the area under the receiver operating characteristic curve (AUC).1
Compared with synovial fluid aspiration, DECT of the feet and ankles demonstrated diagnostic sensitivity of 87%, specificity of 100%, PPV of 100%, NPV of 67%, and AUC of 0.93. Ultrasound of the feet and ankles had a sensitivity of 84%, a specificity of 60%, PPV of 89%, NPV of 50% and AUC of 0.72. Knee DECT had a sensitivity of 91%, a specificity of 87%, PPV of 97%, NPV of 70% and AUC of 0.89. Knee ultrasound had a sensitivity of 58%, a specificity of 80%, PPV of 92%, NPV of 33% and AUC of 0.66.
The use of both DECT and ultrasound at either the feet and ankles or knees increased sensitivity, but lowered accuracy. Using images from both feet and ankles and knees increased sensitivity and NPV, but did not affect accuracy.
This study demonstrated that DECT alone can diagnose gout of either the feet and ankles or knees with a high level of accuracy.
Implications
Although gout is considered bread-and-butter rheumatology, it’s often anything but straightforward. Scenarios exist in which the clinical picture is highly suggestive of a gout flare, but the synovial fluid cannot be successfully obtained, serum and/or synovial fluid chemistries are discordant or equivocal, and/or polarized microscopy does not reveal the presence of monosodium urate crystals. When faced with these clinical conundrums and because we risk misdiagnosis and offering futile and possibly detrimental therapies, should we not strive to use all the tools available to us?
DECT is a non-invasive imaging tool with a remarkable level of accuracy in identifying monosodium urate crystals. Thus, it can provide important diagnostic information when the traditional approach fails. Moreover, it can help detect monosodium urate deposition within atypical sites and anatomic structures that cannot be easily aspirated, such as along entheses.
DECT has the potential to distinguish both acute and chronic forms of gout from some of its common mimickers, such as osteoarthritis (OA) and calcium pyrophosphate dihydrate (CPPD) arthropathy. It can aid the investigation of refractory cases in which other etiologies, such as malignancy, infection and/or subclinical fracture, may exist.
Although further research is needed to assess if DECT can be reliably used on a broader scale to improve medical decision making and patient outcomes, we believe all rheumatology providers should consider the benefits of integrating DECT into their diagnostic algorithm for gout.
Chances in the Tournament
Although there’s some tough competition in the Machine Region and beyond, we strongly believe the final bracket results will crystalize in our team’s favor. DECT promises to be an elegant non-invasive and cost-effective option to accurately diagnose gout—one of the most common conditions we encounter in our rheumatology careers. This potential is especially true in cases in which traditional methods have failed, those that are atypical and those that are refractory to standard treatment.
So what’s there to think about? Bet on DECT in Gout.
Leen Al Saleh, MD, is a first-year rheumatology fellow at MedStar/Georgetown Washington Hospital Center, Washington, D.C.
Ajita Acharya, MD, is a first-year rheumatology fellow at MedStar/Georgetown Washington Hospital Center, Washington, D.C.
Elena Obreja, MD, is a second-year rheumatology fellow at MedStar/Georgetown Washington Hospital Center, Washington, D.C.
Akrithi U. Garren, MD, is a faculty rheumatologist at MedStar/Georgetown Washington Hospital Center, Washington, D.C.
References
- Singh JA, Budzik JF, Becce F, et al. Dual-energy computed tomography vs. ultrasound, alone or combined, for the diagnosis of gout: A prospective study of accuracy. Rheumatology (Oxford). 2021 Oct 2;60(10):4861–4867.
- Bongartz T, Glazebrook KN, Kavros SJ, et al. Dual-energy CT for the diagnosis of gout: an accuracy and diagnostic yield study. Ann Rheum Dis. 2015 Jun;74(6):1072–1077.
 Experience All of RheumMadness
Experience All of RheumMadness
During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports. Check out the reports from each region:
Region: Cells
Region: Animal House
Region: Machines
Region: People
• False Positive MRI in Axial SpA
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The winner of each match-up is decided by a seven-member Blue Ribbon Panel of rheumatologists. The panel will vote based on which topic they think is most important to patients, providers and researchers—both now and in the future. The more your picks match those of the panel, the more points you get. The tournament results will be released in four rounds from March 26–April 4. Prizes will be given to participants with the top scores in the following categories: 1) attending/APP, 2) fellow and 3) resident/medical student. The prize is a custom RheumMadness coffee mug and a lifetime of bragging rights.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn on the RheumMadness website.


