Patient 1: A 59-year-old male initially presented to an emergency department with right wrist drop, and numbness and tingling of his fingers. He had a medical history of hypertension and type 2 diabetes mellitus. He had a prior history of tonsillectomy. Medications included oral hypoglycemics and furosemide. Family history included myelodysplastic syndrome in his mother and coronary artery disease in his father. He worked as an accountant and was married with two children. He smoked one pack per day and had moderate alcohol consumption. Review of symptoms included an unintentional 8 kg weight loss, fatigue, chills, mild dyspnea on exertion, nausea and anorexia.
His vital signs were normal. Physical exam was notable for tanned appearance, hepatosplenomegaly, mild lower extremity edema and right wrist drop with strength of 3 out of 5 during dorsiflexion. Sensory exam was normal, as well as the remaining motor exam.
Laboratory studies revealed hematocrit of 25%, platelet count was 425 x 109 cells per liter (normal <350) and creatinine of 265 μmol/L (from a baseline creatinine of 106 μmol/L). Liver enzymes were normal.
ESR was 107 mm/hour (normal range 1–20). Urinalysis showed no protein, RBCs and WBCs, no granular casts. Peripheral flow cytometry revealed lymphopenia. Serum protein electrophoresis was normal. Tests for antinuclear antibody and anti-neutrophil cytoplasmic antibody were negative. Immunoglobulin G (IgG) subclasses were normal with IgG4 level of 0.390 g/L (normal
Brain MRI was normal, and the patient’s wrist weakness improved throughout his hospital admission. The weight loss, new renal insufficiency and anemia were concerning, and led to further imaging to look for occult malignancy. A CT scan of chest, abdomen and pelvis were abnormal: the main concerns were a T10 sclerotic lesion, multifocal ground-glass opacities of the lungs, as well as diffuse pancreatic enlargement with an intra-abdominal fluid collection (see Figures 1A and B).
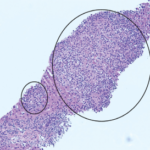
Biopsy of the bone was non-diagnostic, with adequate samples of the pancreas and lung (see Figures 2A and B). Bone marrow biopsy was normal. PET-CT revealed uptake in lung ground-glass opacities, proximal humeri, femoral heads, greater trochanter and head, and body and tail of the pancreas (see Figure 2C).
Intermittent prednisone pulses were initiated by a local oncologist to treat his systemic inflammatory condition. Azathioprine was prescribed between July 2011 and December 2011, until the patient was hospitalized for Legionella pneumonia. He subsequently developed transaminitis, and a liver biopsy revealed nonspecific changes. The lung disease did not resolve, and he was referred to a pulmonologist.