Abdominal MRI showed bilateral hydronephrosis, with abnormalities in the vicinity of the renal pelvis, renal sinuses, and proximal ureters suggestive of either extensive infiltrating carcinoma or retroperitoneal fibrosis (there was abdominal aortic soft-tissue encasement along with renal pelvis, ureter involvement, and rind around the kidneys). Initial rheumatologic evaluation was concerning for ECD; however, differential diagnoses included histiocytosis, amyloidosis, IgG4-RD or idiopathic retroperitoneal fibrosis.
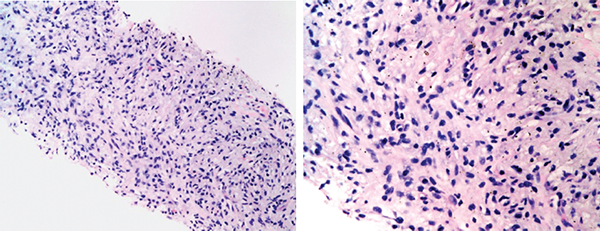
He was hospitalized, and an inpatient CT abdomen showed abnormal soft-tissue attenuation surrounding the infrarenal aorta, inferior vena cava, renal vessels, and ureters causing severe bilateral hydronephrosis and severe bilateral perirenal stranding (see Figures 1C and D, below). There was also an abnormal area of soft-tissue attenuation in the central mesentery. A nonspecific 12 mm lytic lesion in the L2 vertebral body was noted. He underwent placement of nephrostomy tubes and at the same time had laparoscopic biopsy of retroperitoneal tissue. Pathology showed an inflammatory lesion with a lymphohistiocytic infiltrate including foamy histiocytes (see Figure 3A). Immunohistochemical staining showed these histiocytes were positive for CD68 and BRAF and negative for CD1a and S100, most consistent with a diagnosis of ECD (see Figures 3B and C, p. 22). Only rare plasma cells expressed IgG4 (see Figure 3D).
Figures 2C (left) and D (right)
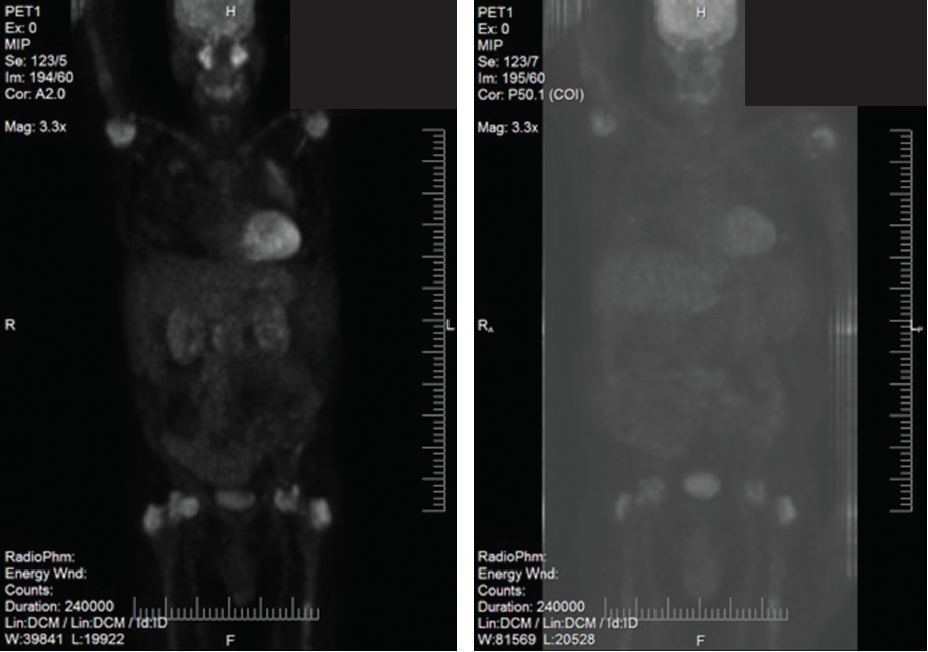
Figures 2A–D show the histopathologic findings and PET-CT findings for Patient 1. 2A and 2B are low- and high-power views (A and B, respectively) of hematoxylin and eosin (H&E) stained lung sections, demonstrating inflammatory infiltration, which includes foamy histiocytes. 2C is a PET-CT prior to treatment with tocilizumab and shows uptake in the lungs, symmetric uptake in proximal humeri, femoral heads and greater trochanter, as well as activity in the head, body and tail of the pancreas. 2D is a PET-CT done at four months of treatment with tocilizumab and shows the lungs with less uptake; no FDG avidity in the pancreas, and stable bone uptake.
TCZ 8 mg/kg IV every four weeks was initiated. His course was complicated by recurrent urinary tract infections. There has been complete resolution of flank pain. A CT scan in January 2016 showed no progression of retroperitoneal soft tissue attenuation around the kidneys, renal veins and aorta. The prominent stranding in the mesentery has decreased compared with his prior CT scan (see Figures 4B and C).
ECD has a male predominance & is typically diagnosed in adults between ages 40 & 70. Diagnosis is often delayed due to its rarity, multiple disease presentations & lack of awareness.
Discussion
We conducted a systematic literature review to expand on the discussion of these two case presentations. Note: We searched the following databases: Scopus, PubMed and Cochrane Library. Our literature search combined the terms Erdheim-Chester disease with treatment. An additional search strategy included Erdheim-Chester disease with tocilizumab.