This group went on to describe a 54-year-old man with ECD who developed a large pericardial effusion.11 He had failed treatment with prednisone, IFN-α and methotrexate (20 mg/wk). Analysis of the exudative effusion demonstrated foamy histiocytes and increased levels of TNFα, CCL2 and IL-6. The intent was to treat with anti-TNFα (infliximab).11
Anakinra, an IL-1 receptor antagonist (IL-1RA), has been reported in a small case series as a treatment for ECD. Aouba et al describe two patients with ECD treated with anakinra.12 The first patient was a 56-year-old female with fever, fatigue, lumbar pain and eyelid xanthelasma, who failed corticosteroids and cladribine. Symptoms resolved on Day 3 with treatment of 100 mg sc/daily anakinra.
Also, a 55-year-old man with similar symptoms responded on Day 5 of anakinra therapy. Interestingly, CRP and IL-6 levels measured at Month 3 dropped significantly. The IL-1β level increased as expected with an IL-1R blocker, but the TNFα levels at Month 3 were unchanged.12 ECD with cardiac involvement has now been treated with anakinra alone, and a case with CNS involvement was treated with anakinra in combination with glucocorticoids.13,14 In the pediatric population, anakinra was used as an effective treatment modality and was subsequently changed to anti-IL-1β therapy with canakinumab every 10 weeks to decrease the frequency of discomfort associated with daily injections.15
BRAF V600 mutations have been reported in 50–100% of patients with ECD, depending on both the series and methods used.16 Vemurafenib, a small-molecule inhibitor of BRAF harboring V600E or, to a lesser extent, V600K mutations, was used in an open series of eight patients with ECD at a dose of 480–960 mg po BID for up to six months. All patients demonstrated a significant reduction of FDG activity on PET.16 Significant side effects included keratosis pilaris, xerosis, photosensitivity and arthralgias. Treatment outcomes are still limited to a handful of cases, and there is no equivalent therapy for patients with wild-type BRAF. Adverse events: Three of the eight patients developed skin cancers, with one patient developing an infiltrative cutaneous squamous cell carcinoma at Month 5.16
Houston et al initially treated a 69-year-old male with biopsy-proven ECD with anakinra to avoid the side effects of IFN, which led to a reduction in pain within two weeks. At that point, molecular studies confirmed BRAF mutation, and anakinra was discontinued in favor of vemurafenib. The patient had return of constitutional symptoms on vemurafenib alone, so anakinra was restarted. The patient’s symptoms resolved rapidly on this combination, which points to a role for combination therapy in the treatment of ECD.17
Back to Our Cases
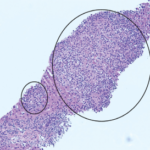
Our two cases of ECD were treated with TCZ as described. Our initial case was treated empirically with TCZ and prednisone based on the assumption that ECD manifestations are largely driven by Th-1 mediated immune response. Further, elevated IL-6 levels have been described in blood and tissues in patients with ECD. Both of our patients had widespread disease with manifestations that were similar to those reported in the literature.27