MikeDotta / shutterstock.com
Higher anxiety levels in postmenopausal women may put them at increased risk of fracture and should be considered when assessing a woman’s risk of osteoporosis as well. This is the conclusion of a study recently published in the journal Menopause that looked at the role of anxiety in bone health.1 Specifically, the study examined the link between anxiety levels and bone mineral density (BMD) and fracture risk among postmenopausal women.
Previous research has focused mainly on the psychological effects of osteoporosis and fracture on quality of life and anxiety levels, according to lead author of the study, Antonino Catalano, MD, PhD, Department of Clinical and Experimental Medicine, University Hospital of Messina, Messina, Italy. Dr. Catalano notes data from this research suggest that “in comparison with healthy women, osteoporotic women show a weakened quality of life and increased anxiety levels.”
What has not been looked at and what is new in this study is how anxiety levels may influence fracture risk. “We looked in the direction from anxiety levels to bone health [in postmenopausal women],” says Dr. Catalano.
The study found higher anxiety levels in postmenopausal women were linked to low bone mineral density and higher fracture risk, independent of other classical risk factors for osteoporosis, such as age, menopausal age, years since menopause and body mass index.
“Our findings suggest a possible new clinical risk factor for osteoporosis that could be measured to improve our ability to identify women at risk for fractures,” says Dr. Catalano.
The Study
The cross-sectional study included 192 white women recruited from a single institution in Messina, Italy. All women underwent evaluation to assess their anxiety level by completing 14 symptom-defining elements of anxiety included in the Hamilton Anxiety Rating Scale (HAMA). These elements include psychological symptoms of anxiety (e.g., tension, fear, sleep and memory issues, and depression), somatic symptoms of anxiety (e.g., aches and pains, ear or eye problems, chest tightness, gastrointestinal symptoms), as well as observed behaviors (e.g., fidgety or restlessness). Based on the results, women were grouped by level from mild (HAMA-1; n=87) to moderate (HAMA-2; n=48) to severe anxiety (HAMA-3; n=57).
All women also underwent evaluation to assess bone mineral density using standard imaging, as well as fracture risk using a computer-based algorithm (i.e., the Fracture Risk Assessment Tool) that calculates the 10-year probability of a major fracture.
The study found the women with the lowest levels of anxiety (HAMA-1) had a significantly lower 10-year probability of a major fracture compared with women who had the highest levels of anxiety (HAMA-3) (20.44% vs. 24.94%, respectively; P=0.03). Women with moderate levels of anxiety (HAMA-2) also had a significantly lower probability of fracture risk than the women with the highest anxiety levels (17.91% vs. 24.94%, respectively; P=0.002).
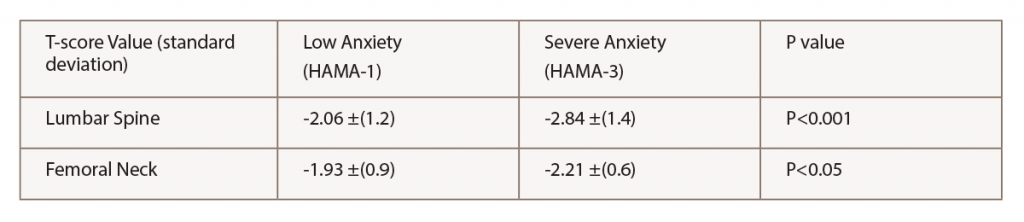
Women with the highest levels of anxiety also had significantly lower BMD than women with the lowest levels of anxiety. When looking at bone density of the lumbar spine and femoral neck, women with the highest anxiety levels had significantly lower T-score values than women at the lowest levels of anxiety (see Table 1).
Dr. Catalano emphasizes the association between high anxiety level and low BMD and fracture risk was independent of other risk factors for osteoporosis in postmenopausal women.
‘Although it’s not necessarily the rheumatologist’s job to treat anxiety, they can recognize & acknowledge the problem, discuss the issue with their patients & make a plan for further evaluation & management.’ —Dr. Pinkerton
Discussion
Commenting on the study, JoAnn V. Pinkerton, MD, executive director, North American Menopause Society, and professor of obstetrics and gynecology, University of Virginia Health System, Charlottesville, Va., underscores how anxiety may influence bone mineral density and fracture risk.
“Women who are anxious have higher cortisol and more markers of inflammation, which appear to induce bone loss by activating bone turnover and, thus, contributes to osteoporosis and fractures,” she says. In addition, she says that anxious women who are restless or fidgety may have lower weight and lower bone mass prior to menopause, placing them at higher risk of fracture once they go through menopause given the subsequent loss of hormones.
Dr. Pinkerton emphasizes the need for primary care physicians and specialty physicians, including rheumatologists, to recognize anxiety in their patients.
“Although it’s not necessarily the rheumatologist’s job to treat anxiety, they can recognize and acknowledge the problem, discuss the issue with their patients and make a plan for further evaluation and management through either the patient’s primary care physician or referral to a mental health specialist,” she says.
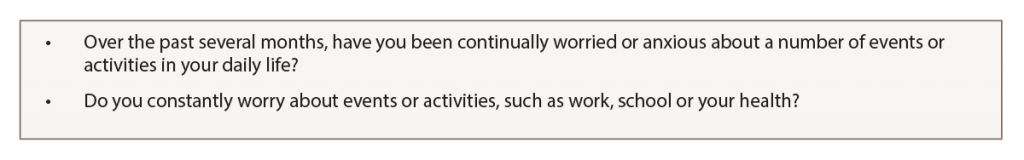
Asking some simple questions can help identify patients who are anxious (see Table 2).
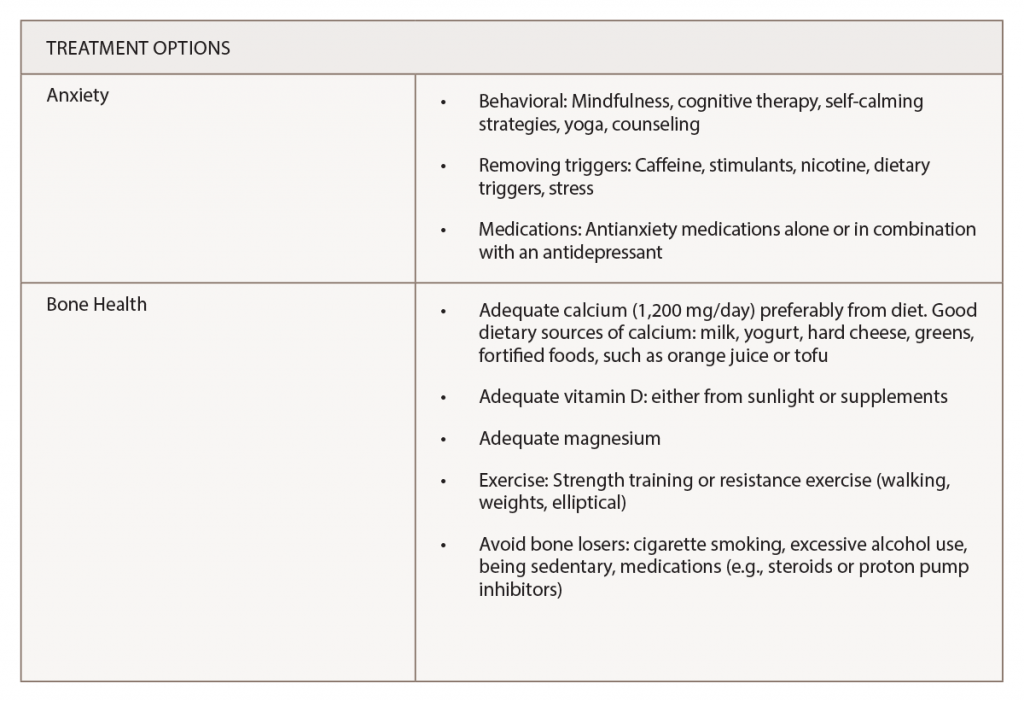
In addition, Dr. Pinkerton highlights a number of treatment options for anxiety, as well as ways to maintain good bone health in perimenopausal and menopausal women (see Table 3).
For Dr. Catalano, focusing on the effect of anxiety on bone health provides physicians with another way to identify women at risk of osteoporosis and fracture.
“By our results, we hope to improve the physician’s ability to recognize postmenopausal women at higher risk of osteoporosis and related fractures to improve early diagnosis and prevent the first fracture,” he says.
He also emphasizes the need for physicians to consider fracture risk assessment in postmenopausal women with higher anxiety levels.
Mary Beth Nierengarten is a freelance medical journalist based in Minneapolis.
Reference
- Catalano A, Martino G, Bellone F, et al. Anxiety levels predict fracture risk in postmenopausal women assessed for osteoporosis Menopause. 2018; 25(10). doi: 10.1097 GME.0000000000001123. [Epub ahead of print]