Want to know more about vasculitis in the nervous system? Check out these abstracts from Arthritis & Rheumatism, and log on to www.wileyonlinelibrary.com/journal/arthritis to read the full articles.
Giant cell arteritis: Involvement of intracranial arteries. (Arthritis Rheum. 2006; 55:985-989.)
Introduction
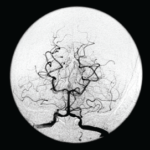
Cerebrovascular ischemic events have been reported in 3% to 4% of patients with giant cell arteritis (GCA). Clinical and pathologic findings suggest that these ischemic events are due to involvement of extradural vertebral and carotid arteries with high-grade stenosis or occlusion rather than intracranial vasculitis.
Several previous reports have described patients with cerebral vasculitis who were also considered to have GCA. However, most of these patients probably represent cases of primary central nervous system vasculitis (PCNSV), a different disease with similar histopathologic findings. To determine the occurrence and frequency of central nervous system (CNS) vasculitis in GCA, we reviewed the medical records of all patients with a diagnosis of CNS vasculitis or angiitis at the Mayo Clinic (Rochester, MN) over a 17-year period and identified those with both biopsy-proven GCA and pathologic and/or angiographic evidence of intracranial vasculitis.
Primary central nervous system vasculitis with prominent leptomeningeal enhancement: A subset with a benign outcome. (Arthritis Rheum. 2008; 58:595-603.)
Abstract
Objective: Primary central nervous system vasculitis (PCNSV) is an uncommon condition that affects the brain and spinal cord. This study was undertaken to evaluate the clinical features and outcomes among patients with PCNSV who presented with prominent gadolinium meningeal enhancement on magnetic resonance imaging (MRI).
Methods: Through retrospective review using the Mayo Clinic medical records linkage system, we identified 101 consecutive patients with PCNSV based on brain biopsy or conventional angiography (or both) between January 1, 1983 and December 31, 2003. We evaluated data on demographics, clinical findings, laboratory studies, imaging, biopsy of brain or spinal cord (or both), treatment, and neurologic outcome.
Results: MRIs showed prominent leptomeningeal enhancement in eight of 101 patients with PCNSV. In six of those eight, cerebral angiography or magnetic resonance angiography results were normal, but biopsy of the brain or spinal cord showed vasculitis in all eight. Granulomatous vascular inflammation was found in six specimens and was associated in four cases with vascular deposits of beta-amyloid peptide. All eight patients had a prompt response to therapy, with resolution of the MRI meningeal enhancement. Although three of the eight patients had relapses during followup, the overall outcome was favorable. Patients with meningeal enhancement, compared with patients without enhancement, more commonly had substantial abnormalities of cerebrospinal fluid (100% versus 58%; P=0.02) and amyloid angiopathy (50% versus 12%; P=0.03).
Conclusion: Prominent gadolinium leptomeningeal enhancement on MRI may point to a distinct subtype of PCNSV with small leptomeningeal artery vasculitis and rapid response to therapy.
Primary central nervous system vasculitis in children. (Arthritis Rheum. 2006;54:1291-1297.)
Abstract
Objective: Primary angiitis of the central nervous system (PACNS) is a severe and ill-defined neurologic disease. The goal of this study was to characterize the presenting features, treatment, and neurologic outcome of PACNS in children (cPACNS) and to define the predictors of disease progression in order to identify high-risk patients with cPACNS.
Methods: The cohort comprised consecutive patients diagnosed as having cPACNS based on clinical and vascular imaging findings, including identification of arterial stenosis on conventional angiography or magnetic resonance (MR) angiography. Disease progression was defined angiographically at more than three months after initial angiography. Clinical data obtained in prospectively collected standardized assessments and results of laboratory tests, including detection of cerebrospinal fluid abnormalities, were noted, and neuroimaging studies were reanalyzed. Predictors of progression were identified and tested in multivariate regression models.
Results: Sixty-two consecutive patients with cPACNS (38 male, 24 female, median age 7.2 years) were included. Two distinct subgroups were identified, those with progressive disease and those with nonprogressive disease. Progressive cPACNS was found in 20 of 62 children and was predicted by a clinical presentation of neurocognitive dysfunction, multifocal parenchymal lesions on MR imaging, and evidence of distal stenoses on angiography.
Conclusion: The spectrum of PACNS in children includes both progressive and nonprogressive forms. Characteristic features at diagnosis can be used to predict later progression, to identify a distinct high-risk cPACNS cohort, and to help guide selection of patients for immunosuppressive therapy.
Efficacy of tumor necrosis factor alpha blockade in primary central nervous system vasculitis resistant to immunosuppressive treatment. (Arthritis Rheum. 2008;59:291-296.)
Introduction
Primary central nervous system vasculitis (PCNSV) is an uncommon form of vasculitis that is limited to the brain and spinal cord. PCNSV may be associated with serious morbidity and mortality unless it is treated with high-dose corticosteroids and immunosuppressive medications.
Because of the lack of controlled clinical trials and uniform diagnostic criteria, uncertainties exist regarding the response to treatment and the long-term outcome of PCNSV. Some patients may have a more benign course and may need less intense therapy. Others require more aggressive therapy. Still others experience recurrent symptoms or have severe adverse effects, therefore new treatment options are needed.
We report two patients with PCNSV who did not respond to treatment with corticosteroids and immunosuppressive medication. They were treated with tumor necrosis factor (TNF) blockers in an attempt to control the disease. This study was approved by the Mayo Clinic Institutional Review Board.
Angiography-negative primary central nervous system vasculitis in children: A newly recognized inflammatory central nervous system disease. (Arthritis Rheum. 2005;52:2159-2167.)
Abstract
Inflammatory central nervous system (CNS) diseases in childhood comprise a wide spectrum of heterogeneous conditions. We studied four children with primary CNS vasculitis in whom results of magnetic resonance imaging studies were abnormal but results of conventional angiography were normal. We determined that angiography-negative, biopsy-confirmed primary small-vessel CNS vasculitis is a previously unrecognized distinct disease entity in children. The diagnosis must be considered in a child with a progressive, acquired diffuse or focal neurologic deficit, even if the results of conventional angiography are normal. A lesional brain biopsy is required to confirm the diagnosis. Use of immunosuppressive therapy plus aspirin leads to an excellent neurologic outcome.
Primary central nervous system vasculitis presenting with intracranial hemorrhage. [abstract]. (Arthritis Rheum. 2010;62(Suppl 10):2037.)
Objective: Primary central nervous system vasculitis (PCNSV) is an uncommon and heterogeneous condition that affects the brain and spinal cord. This study was undertaken to evaluate the clinical features and outcomes of patients who presented with intracranial hemorrhage (IH) in the context of the largest cohort of consecutive patients with PCNSV studied to date.
Methods: We identified 131 consecutive patients with PCNSV seen over the 25-year period of 1983 to 2007. PCNSV diagnoses were based on findings from a central nervous system (CNS) biopsy or conventional angiography (or both). We compared patients presenting with IH (within three months of the date of PCNSV diagnosis) to those without. We evaluated data on demographics, clinical findings, laboratory studies, imaging, biopsy of brain or spinal cord (or both), treatment and neurologic outcome.
Results:Sixteen (12.2%) cases had IH at presentation. Twelve patients had intracerebral hemorrhage (ICH), and four subarachnoid hemorrhage. Cerebral angiography was performed in 13 patients and showed multiple-vessel vasculitic changes in all. CNS biopsy findings were positive in four patients. Three patients had an acute necrotizing pattern, one had a granulomatous inflammatory pattern. Amyloid angiopathy was observed in 2 biopsy-positive specimens.
Compared with the 115 patients without, the 16 patients presenting with IH were more frequently females (100% versus 50.4%, p<0.001), persistent neurological deficit or stroke (12.5% versus 42.6%, p=0.027) and altered cognition (25% versus 56.5%, p=0.030) occurred less frequently, and the frequency of patients who had discontinued therapy by the last follow-up visit was higher (37.5% versus 14.2%, p=0.031). MRI and angiographic findings (excepted the presence of ICH), type of therapy (corticosteroids only or associated to immunosuppressive agents), therapy duration, frequencies of relapses, cerebrospinal fluid abnormalities, and Rankin disability score at last follow-up were similar. The survival curves of patients with and without IH were not different.
Conclusion: IH is not a rare presenting finding of PCNSV. These patients are predominantly females. The higher frequency of patients not requiring therapy at last follow-up suggests a more favorable response to therapy. An association with amyloid angiopathy may be present.