Want to learn more about bisphosphonates and fractures? Check out these abstracts from Arthritis & Rheumatism and Arthritis Care & Research, and log on to www.wileyonlinelibrary.com/journal/arthritis to read the full articles.
Hip fracture patients are not treated for osteoporosis: A call to action.
(Arthritis Care Res. 2002; 47:651–654.)
Abstract
Objective: To determine whether hip fracture patients, a group at very high risk for additional fragility fractures, are being evaluated and treated effectively for osteoporosis.
Methods: Clinical and bone densitometry (dual X-ray absorptiometry [DEXA]) records were reviewed in hip-fracture patients at 4 Midwestern US health systems to determine the frequency of DEXA use, calcium and vitamin D supplementation, and antiresorptive drug treatment.
Results: DEXA was performed at the four study sites in only 12%, 12%, 13%, and 24% of patients, respectively. Calcium and vitamin D supplements were prescribed in 27%, 1%, 3%, and 25% of the patients at the four study sites. Antiresorptive drugs were prescribed in 26%, 12%, 7%, and 37% of the patients with only 2–10% receiving a bisphosphonate.
Conclusion: Reducing osteoporotic fractures will require more effective approaches to managing hip-fracture patients and other high-risk populations.
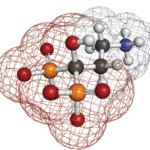
Fracture risk before and after total hip replacement in patients with osteoarthritis: Potential benefits of bisphosphonate use.
(Arthritis Rheum. 2011;63:992–1001.)
Abstract
Objective: The association between osteoarthritis (OA) and fractures remains unclear. OA patients have increased bone mass, but no corresponding decrease in fracture rate. This study was undertaken to determine the fracture rates in patients with hip OA undergoing a total hip replacement (THR), as compared with disease-free controls, and to assess the association between bisphosphonate use and postsurgery fracture risk.
Methods: We conducted a population-based parallel-cohorts study. All patients in the UK General Practice Research Database undergoing a THR for hip OA between 1986 and 2006 constituted the exposed cohort (n = 14,133). Five disease-free controls were matched with each patient by age, sex, and practice site. Subjects were followed up for 5 years before and after surgery. Fracture rates and rate ratios (RRs) were estimated using Poisson regression. In addition, bisphosphonate use was identified among patients undergoing THR, and the data, stratified by the presence or absence of a previous fracture and by treatment propensity score, were assessed using fitted Cox models to study the effect of bisphosphonate use on the risk of fracture postsurgery.
Results: Patients undergoing a THR had a similar fracture risk as that in controls in the 5 years before THR, but had higher rates postsurgery, which peaked at years 2.5–5 (adjusted RR 1.24, 95% confidence interval [95% CI] 1.02–1.52). Use of bisphosphonates lowered the fracture risk among THR patients who received bisphosphonates as primary prevention (hazard ratio [HR] 0.56, 95% CI 0.38–0.82) and also among THR patients who had experienced a previous osteoporotic fracture (HR 0.48, 95% CI 0.23–0.99).
Conclusion: This study identified a 25% increase in fracture risk at 2.5–5 years postsurgery among patients undergoing a THR. Bisphosphonate use reduced the post-THR risk of fracture when administered both as primary prevention and as secondary prevention, by 44% and 52%, respectively. This must be further confirmed in randomized controlled trials.