Victor Moussa / shutterstock.com
The opioid epidemic in the U.S. has destroyed thousands of lives and torn families apart. According to the Centers for Disease Control and Prevention, an average of 130 people in the U.S. die each day from an opioid overdose. From 1999 to 2017, more than 700,000 died as a result of drug overdoses. In 2017, the number of overdose deaths involving opioids (both legal prescription and illegal opioids, such as heroin) was six times higher than in 1999.
Three distinct waves have defined the increase in opioid overdose deaths. The first wave began in the 1990s and resulted from increased prescriptions by healthcare providers. Overdose deaths involving prescription opioids (natural and semisynthetic opioids and methadone) have increased steadily since 1999. The second wave began in 2010 and was marked by rapid increases in overdose deaths attributable to heroin. The third wave began in 2013 with significant increases in overdose deaths attributable to synthetic opioids, particularly those involving illicitly manufactured fentanyl.
In 2017, the U.S. Department of Health & Human Services declared a public health emergency and announced a five-point strategy to combat the opioid crisis:
- Improve access to treatment and recovery services;
- Promote the use of overdose-reversing drugs;
- Strengthen understanding of the epidemic through better public health surveillance;
- Provide support for cutting-edge research on pain and addiction; and
- Advance better practices for pain management.
In 2018, the SUPPORT for Patients and Communities Act was passed. This legislation reforms Medicare and Medicaid to better help patients with opioid addictions and promotes national education regarding the risks associated with opioid use.
Many states have also taken action to help reduce the number of opioid overdose deaths. A handful of states now require patients seeking opioid medication for chronic pain to enter into a contract with their providers before a prescription is written. However, a growing school of thought indicates these contracts may do more harm than good.
What Is an Opioid Contract?
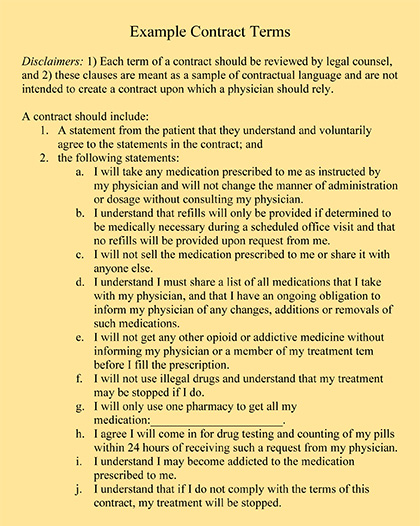
The purpose of an opioid contract is to provide information regarding the pros and cons associated with opioid use. A contract is intended to deter abuse, improve the positive outcomes associated with opioid use and minimize the prescribing physician’s risk. As part of the contract, patients must agree to undergo random urine drug screens and pill counts, and to receive opioid prescriptions only from the physician identified in the contract.
By signing, patients agree to abide by the dosing and frequency prescribed, participate in certain programs, not request opioids or other pain medicine from other physicians, participate in mental health assessments if necessary and, to the extent possible, obtain all medications from one pharmacy. The contract typically includes a list of actions that would permit the physician to stop prescribing opioids or change the treatment plan. Finally, the contract usually includes a description of safety risks, potential side effects and tips for medication management.
In short, a contract ensures:
- The risk of prescription opioid misuse is minimized;
- The harmful effects associated with opioid use are communicated to the patient;
- A deterrent to self-medicating and drug-seeking behavior is provided; and
- Consistent medical care is provided, irrespective of race or financial status.
Harmful Effects
Despite the contract’s best intentions, many providers find opioid contracts do more harm than good. There is questionable evidence regarding whether the agreements actually reduce opioid misuse in patients with chronic pain. Additionally, many patients complained their stress and anxiety increased as a result of the agreement due to concerns associated with fulfilling its terms.
Some patients who claimed they had no substance abuse issues feared a mistake would lead to their urine sample testing positive for drugs it should not or testing negative for drugs for which it should test positive. These patients feared they would lose the pain medication they have come to rely on.
Further, some physicians and patients feel the agreements cause the physician–patient relationship to break down. Instead of a way to carefully navigate a complicated medical problem, the contract becomes the foundation for treatment, and if violated, the treatment abruptly ends.
Improving the Effect of Opioid Agreements
Whether a physician agrees with the use of opioid agreements or is legally obligated to enter into them under state law, certain measures can be taken to enhance the positive effect of the agreements. These measures include:
- Carefully drafting the agreement using plain language that is easily understood by the patient. Forcing patients to sign a document loaded with legalese can negate the whole purpose of the agreement;
- Taking time to calmly walk the patient through the terms of the agreement so he or she understands the expectations and is aware of all actions that could impact treatment;
- Periodically reviewing the terms of the agreement with each patient to confirm they continue to understand and abide by the expectations and responsibilities agreed to; and
- For patients violating the terms of the agreement, weaning the patients off the medication, if permitted, instead of completely cutting them off.
 Steven M. Harris, Esq., is a nationally recognized healthcare attorney with McDonald Hopkins LLC. Contact him via email at [email protected].
Steven M. Harris, Esq., is a nationally recognized healthcare attorney with McDonald Hopkins LLC. Contact him via email at [email protected].