Abstract 0224 presented at ACR Convergence 2024
Background/Purpose
Magnetic resonance imaging (MRI) of the sacroiliac joints is widely used for diagnosing and monitoring patients with spondyloarthritis (SpA). However, local radiologists may be less familiar [than rheumatologists] with assessing MRIs in patients with spondyloarthritis potentially leading to misinterpretations and affecting the final diagnosis. We compared assessments of sacroiliac joint MRIs in patients with a diagnosis of axial spondyloarthritis (axSpA) or psoriatic arthritis (PsA) in local MRI reports from routine care in five European countries with re-reads by central experts to estimate the extent of over- or under-reporting of features and misclassification.
Methods
We included patients with a diagnosis of axSpA or PsA in a clinical patient registry from one of five European countries (DANBIO, Denmark; SCQM, Switzerland; ATTRA, Czech Republic; biorx.si, Slovenia; ICEBIO, Iceland; all participating in the EuroSpA Research Collaboration Network) with an available MRI of the sacroiliac joints and a corresponding local MRI report. MRIs were collected and read centrally by two experienced readers, blinded to clinical (except sex and age) and other imaging information. Readers registered whether the MRI was overall indicative of axSpA. In case of disagreement, MRIs were adjudicated by an experienced musculoskeletal radiologist (member of the ASAS/EULAR MRI group). Further, presence/absence of inflammatory and structural lesions (details in Table 1) were registered. Similar information was extracted from the local reports. Findings in local reports and central assessments were compared using central reads as reference standard.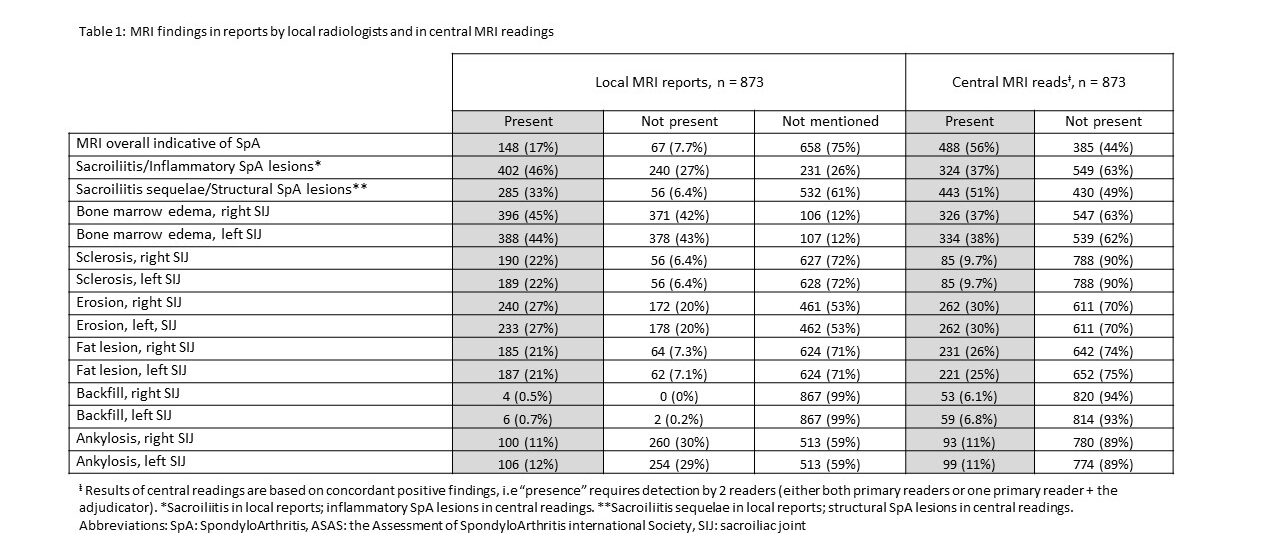
Results
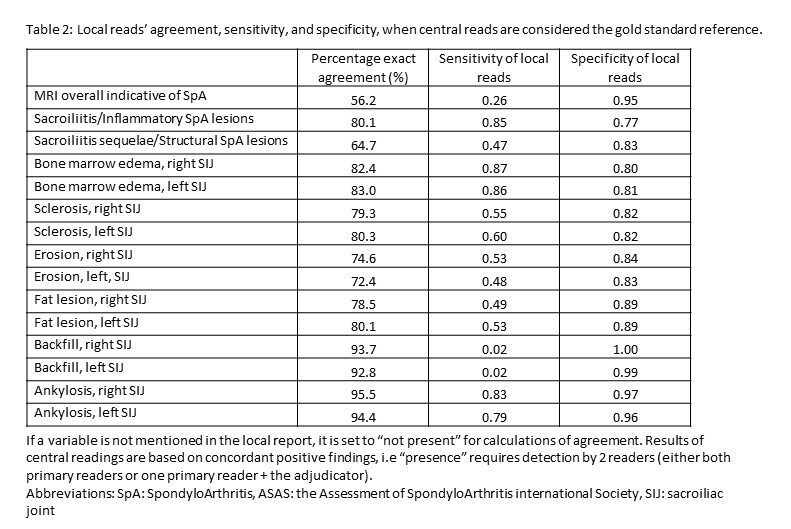
Overall, 873 patients with an MRI of the sacroiliac joints and a corresponding local MRI report were included; mean age 37.9 years, 475 (54%) male and 704/169 diagnosed with axSpA/PsA (see Table 1). Sacroiliitis/inflammatory SpA lesions were reported more often in local vs central reads (46% vs. 37%). Sacroiliitis sequelae/structural SpA lesions were reported less often in local vs. central reads (33% vs. 51%). In 17% of cases, local reads explicitly reported if the MRI was overall indicative of axSpA or not. On lesion level, bone marrow edema was the most frequent lesion judged present, both in local and central reads (right/left joint 45%/44% vs. 38%/37%, respectively), followed by erosion (27%/27% vs. 30%/30%). Compared with central reads, local reads tended to overestimate presence of bone marrow edema and sclerosis, underestimate/not assess backfill, while the frequency of erosions, fat and ankylosis was similar. Figure 1 shows examples with disagreement.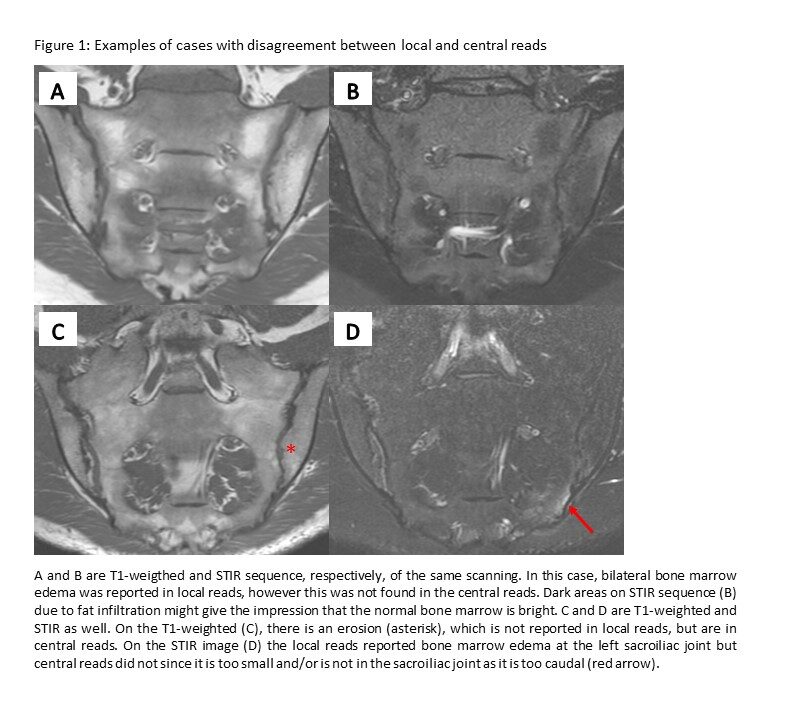 The sensitivity and specificity of local reads were 0.85 and 0.78 for sacroiliitis/inflammatory SpA lesions, and 0.48 and 0.83 for sacroiliitis sequelae/structural SpA lesions, respectively (see Table 2). For individual lesions, the sensitivity of local reads was highest for BME and ankylosis, followed by sclerosis. The specificity of local reads was ≥0.80 for all lesions.
The sensitivity and specificity of local reads were 0.85 and 0.78 for sacroiliitis/inflammatory SpA lesions, and 0.48 and 0.83 for sacroiliitis sequelae/structural SpA lesions, respectively (see Table 2). For individual lesions, the sensitivity of local reads was highest for BME and ankylosis, followed by sclerosis. The specificity of local reads was ≥0.80 for all lesions.