
Kami Schmidt (seated at lower left) with the East Central Minnesota Vasculitis Support Group in Minnesota.
Ms. Brechtelsbauer’s vasculitis began in 2009 with diffuse urticaria, but it took doctors several years to diagnose it, even though a skin biopsy revealed high eosinophil counts. She developed asthma, and then eosinophilic pneumonia. She tested negative for anti-neutrophil cytoplasmic antibodies (ANCA) but has since learned that only half of all patients have them.
At one point, she said, “I was on 10 different medications just to breathe,” she said. She was getting high-dose prednisone and finally began to improve a bit when doctors put her on omalizumab (Xolair). Even so, she endured five surgeries over five years. In the midst of one of them, she developed a new allergy to the anesthesia that nearly killed her. When she went into cardiac arrest, doctors had to perform CPR for two minutes to resuscitate her.
At a June 2015 vasculitis conference in Jacksonville, Fla., she had heard about promising new results from mepolizumab. When the FDA approved the drug in November 2015 to treat adults with eosinophilic asthma, “I was in my doctor’s office the next week, saying, ‘I want this,’” she recalled. “I knew about the Nucala approval before my immunologist.”
The combination of omalizumab and mepolizumab has “done wonders” for her EGPA as well, she said, and finally allowed her to taper off prednisone. “I’ve got a great team now,” she said, but she noted that she shopped around and assembled the providers on her own. Nevertheless, Ms. Brechtelsbauer said she feels lucky to be alive. “Right now, I’m doing great,” she said. “Biologics saved my life.” In addition to her wife and caregiver, Cheryl, she said, Facebook groups, national meetings and the Vasculitis Foundation have been strong pillars of support, especially given her ultra-rare disease. “To find your little tribe within that is amazing,” she said.
Advances on 3 Fronts
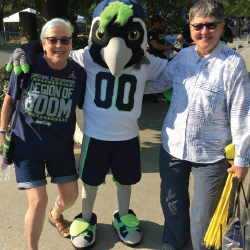
Rosemary Brechtelsbauer (left) and her wife, Cheryl (right) enjoying life at a Seattle Seahawks football game with the mascot.
In his opening talk, Dr. Seo grouped the emerging vasculitis therapies into three main categories: selective immune cell depletion, cytokine-based strategies and inhibition of immune targeting. Rituximab, in the first category, is a monoclonal anti-CD20 antibody that destroys B cells tagged with the CD-20 cell surface marker. B cell strategies are now standard for the treatment of both MPA and GPA (granulomatosis with polyangiitis). The two forms of ANCA-associated vasculitis attack small blood vessels, mainly in the lungs and kidneys. Rituximab received FDA approval to treat both conditions in 2011, and the drug is now used to treat cryoglobulinemic vasculitis, as well.
The second main treatment category, cytokine-based strategies, can “prevent the immune system from ganging up on you,” Dr. Seo said. Because cytokines instigate immune cells, targeting them can prevent a misguided attack. The pro-inflammatory cytokine IL-6, for example, spurs the production of infection-
fighting cells and proteins.
Mepolizumab works in much the same way by targeting interleukin (IL) 5, which Dr. Seo called “Miracle-Gro for eosinophils.” Weeding out eosinophils can knock back EGPA.
Giant cell arteritis (GCA), associated with blindness and stroke, may respond to anti-IL-6 inhibition. Tocilizumab (Actemra) gets rid of IL-6, and a phase 3 clinical trial (GiACTA) concluded that GCA patients on the drug were much less likely to flare as they tapered prednisone use, compared to patients on prednisone and a placebo.1 In response, the FDA approved tocilizumab for GCA in 2017. Not everyone has benefited: clinical trial data suggest that tocilizumab has been less effective in treating Takayasu’s arteritis, a large vessel vasculitis seen more often in younger women.
The third treatment category relies on inhibition of immune targeting, such as blocking or eliminating the antibodies used by the immune system to tag and attack blood vessels. “They can’t hurt you if they can’t find you,” Dr. Seo said. Recent reports from a large multinational study, PEXIVAS, suggest that plasmapheresis, or removing antibodies via plasma exchange, wasn’t effective in significantly reducing mortality or the risk of end-stage renal disease among ANCA-associated vasculitis patients, although the investigators stress the analysis is not yet complete.
Dr. Seo noted that researchers have reported more success, at least thus far, in getting rid of other immune tags, such as the protein fragment C5a. The phase 2 CLEAR trial tested a new ANCA-associated vasculitis drug candidate, Avacopan, which Dr. Seo compared with “Teflon for your blood vessels.” By preventing the C5a tag from sticking to them, researchers hypothesized that it could help eliminate the condition. In the CLEAR study, researchers reported that Avacopan plus standard medications did significantly better in getting patients into rapid remission than standard medications alone.
Better yet, Dr. Seo said, the drug may work without steroids—a statement that drew appreciative oohs from the audience. Steroids are “what make you cranky and want to throw toasters at people and tell them what you really think about them,” he said, to laughter and vigorous nodding. From an efficacy standpoint, he concluded, Avacopan may yet give rituximab a run for its money.
The PEXIVAS study likewise suggested high-dose oral glucocorticoids were no better than low-dose steroids in further improving the outcomes of patients treated with cyclophosphamide or rituximab. In other words, Dr. Seo said, the drugs have opened the possibility, for the first time, of treating vasculitis with much less or even no steroids. That assessment was especially popular with the audience.
In response to questions, Dr. Seo cautioned that rituximab carries a small but potentially serious risk for common variable immune deficiency (CVID), a disorder linked to low immunoglobulin levels that can disrupt someone’s ability to produce new antibodies. “It’s not a slam dunk to remain on rituximab forever,” he said.


