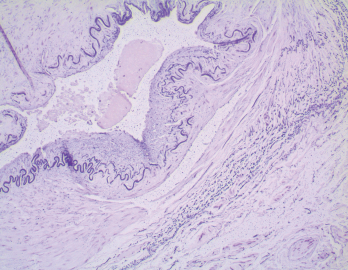
Figure 2. In the biopsy of the right temporal artery with elastin staining, the internal elastic lamina is preserved despite the appearance of artifactual interruptions in the internal elastic layer caused by specimen processing.
She was started on gabapentin for presumptive right-sided occipital neuralgia. Her headaches persisted but were less severe.
One day after she discontinued prednisone, she awoke with diplopia and right eye ptosis, prompting her to return to the emergency department. This is when we met the patient.
Her exam revealed a pupil-involving, partial, right third cranial nerve palsy. She had a partial ptosis, medial rectus palsy and non-reactive pupil. Her left superficial temporal artery was indurated. Her laboratory tests were again significant for a marked elevation in her inflammatory markers (ESR: 86 mm/hr; CRP:186 mg/L).
The differential diagnosis of a severe headache and third nerve palsy includes aneurysmal third nerve involvement, microvascular ischemic cranial neuropathy, inflammatory meningitis as in neurosarcoidosis, carcinomatous meningitis and GCA.
Computed tomography angiography (CTA) of the head and neck was performed, and MRI of the brain and orbits was also obtained. The head CTA showed no evidence of aneurysm. The neck CTA showed an irregularity of the external carotid arteries on both sides, raising concern for vasculopathy.
The patient underwent a lumbar puncture, and the analysis of the cerebrospinal fluid (CSF) was unrevealing. Her third nerve palsy, new headache, elevated ESR/CRP, and imaging findings made us most suspicious for GCA.
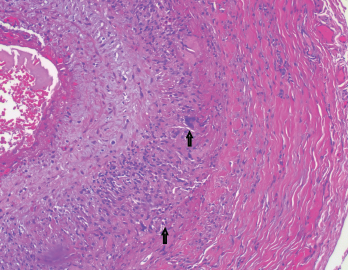
Figure 3. The biopsy of the left temporal artery with H&E staining shows multinucleated giant cells.
She was started on 1,000 mg of intravenous methylprednisolone daily. A left temporal artery biopsy was performed the next day (see Figures 3&4, opposite). Her symptoms began to improve within hours of starting the intravenous steroids, and all of her symptoms resolved within 48 hours.
The left temporal artery biopsy showed full-thickness inflammation of the vessel involving the intima, media and adventitia. The inflammatory cells included eosinophils, lymphocytes, scattered neutrophils and many multinucleated giant cells. The pathology was consistent with a diagnosis of GCA.
After receiving intravenous methylprednisolone for three days, she was started on 1 mg/kg of oral methylprednisolone. The dose was tapered gradually, according to GCA treatment protocols.
She had side effects of severe insomnia, facial swelling and moderate weight gain after starting steroid therapy. She refused to start tocilizumab initially because she was concerned about the potential side effects.
Her right-sided headaches recurred on two occasions when she was tapered to 12 mg per day of methylprednisolone and improved quickly when the dose was raised back to 16–20 mg per day.
At this point, our patient agreed to start tocilizumab therapy. It was administered as monthly intravenous infusions at a dose of 8 mg/kg. After she started tocilizumab, the methylprednisolone dose was able to be decreased rather rapidly.
Six months after her diagnosis, she was down to 4 mg per day of methylprednisolone. She remained asymptomatic with normal inflammatory markers.

