 When coding evaluation and management (E/M) services provided to a patient, one of the most persistent concerns is whether a patient is new or established to the practice. Although this may seem like a simple coding answer, the distinction is an important one, because it enables providers to appropriately bill and receive reimbursement correctly. E/M service is a key factor in rheumatology practices and it is imperative that your coding hold up to any claims review to prevent payment delays.
When coding evaluation and management (E/M) services provided to a patient, one of the most persistent concerns is whether a patient is new or established to the practice. Although this may seem like a simple coding answer, the distinction is an important one, because it enables providers to appropriately bill and receive reimbursement correctly. E/M service is a key factor in rheumatology practices and it is imperative that your coding hold up to any claims review to prevent payment delays.
In 2012, the Current Procedural Terminology (CPT) manual made subtle changes to the definition of a new patient; unfortunately, the Centers for Medicare & Medicaid Services (CMS) did not change its definition to stay aligned with these updates. This discrepancy, along with the complex rules and regulations of E/M, has caused great confusion for many providers and their compliance efforts.
New vs. Established Patients
Keep in mind, not all E/M codes are categorized as new or established patients, such as initial observation care, critical care services, emergency department, inpatient consultations, etc. For example, patients seen in the emergency department are always defined as new, and the provider is expected to record the patient’s history at all times to diagnose a problem. For purposes of billing for E/M services in the office setting, patients are identified as either new or established, depending on face-to-face encounter(s) with a provider. The patient distinction is important in the office setting, since new patient codes carry higher relative value units based on the additional work new patient visits require.
The CPT manual differentiates new and established patients:
- A new patient is one who has not received any professional services from the physician/qualified healthcare professional or another physician/qualified healthcare professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years. The CPT code group is 99201-99205.
- An established patient is one who has received professional services from the physician/qualified healthcare professional or another physician/qualified healthcare professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years. The CPT code group is 99211-99215.¹
However, the CMS has different definitions of new and established patients in the Medicare Claims Processing Manual, Chapter 12—Physician/Nonphysician Practitioners, Section 30.6.7:
- Interpret the phrase “new patient” to mean a patient who has not received any professional services (i.e., E/M service) or other face-to-face service (e.g., surgical procedure) from the physician or physician group practice (same physician specialty) within the previous three years. For example, if a professional component of a previous procedure is billed in a three-year time period (e.g., a lab interpretation) is billed and no E/M service or other face-to-face service with the patient is performed, then this patient remains a new patient for the initial visit. An interpretation of a diagnostic test, reading an X-ray or EKG, etc., in the absence of an E/M service or other face-to-face service with the patient does not affect the designation of a new patient.²
Understanding the three components and awareness of the rules are necessary to bill for new patients. Let’s take a look at each component:
Professional services: This term can be interchangeable with the term physician services. Professional and/or physician services are face-to-face services, which include office visits, surgical procedures and a broad range of other diagnostic and therapeutic services. These services are furnished in all settings, including physician offices, hospitals, other post-acute care settings and clinical laboratories. For example, suppose the provider reviews a diagnostic image or lab for an inpatient he/she did not actually meet in person and the patient is requested to see the rheumatologist upon discharge. At the visit, the rheumatologist bills a new patient visit because there was no face-to-face encounter during the inpatient stay.
Three-year rule: The general rule for all payers in determining if a patient is new is that a previous, face-to-face service must have occurred at least three years from the date of service. For example, a patient is seen in the office on May 7, 2015. He moves to the other side of town and has recently moved back in the area and makes an appointment with the office to see the rheumatologist on May 8, 2018. Because it has been a full three years since his last date of service, the office will bill this as a new patient visit.
Different specialty/subspecialty with the same group: This area continues to cause confusion when billing for a patient who is seen by different providers within the same group. This goes back to how the practice bills for services. If everything is billed under one tax identification number (especially for group practices), even if a patient is referred to a specialist, this must be billed as an established patient.
Multiple practice sites, same tax identification number: Consider the scenario in which a group practice has multiple sites of care, all billing under the same tax identification number, and each site has their own patient records that are not available at other clinic sites. A patient is a regular at clinic site A, but was sent to clinic site B to be evaluated by a different physician or non-physician provider (NPP) who has never seen the patient and has no records available. Should this patient be coded as a new patient or an established patient? If a patient has been seen in the previous three years by any physician or NPP in the same group and specialty, regardless of which clinic site they went to and regardless of whether patient records are available, only established patient codes should be used. CMS and CPT rules do not provide exceptions to practice sites that do not have access to records.
Get It Right
Although new and established patient visits seem easy enough to distinguish, understanding the definition and coding correctly are vital to a practice’s bottom line. There are important differences between the codes: New patient visit codes (99201–99205) require all three key components (history, exam and medical decision making) to be satisfied in the documentation, although the established patient codes (99211–99215) require only two of the three key components.
With the updates to CPT definitions and payer guidelines, the reason for learning to distinguish new patients from established patients, apart from following coding guidelines, is that it enables practices to be more efficient and effective with appropriate reimbursement for patient visits, while also minimizing audits and other payer scrutiny.
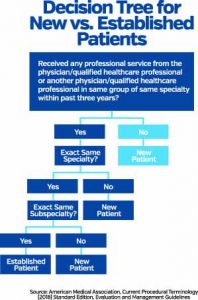
See the decision tree graphic above for determining if a patient is new or established. For additional questions or information on coding and billing training, contact the ACR coding and practice management department at [email protected].
References
- Current Procedural Terminology (CPT) 2018. American Medical Association.
- Medicare Claims Processing Manual (Chapter 12)—Physicians/Nonphysician Practitioners (30.6.7).

