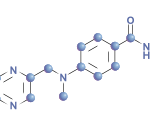
Baricitinib is a once-daily oral Janus kinase 1 (JAK1)/JAK2 inhibitor in development to treat patients with moderate to severe rheumatoid arthritis (RA). Because many patients who suffer from chronic inflammatory rheumatic diseases may also have comorbidities, physicians have asked whether baricitinib is an effective treatment in these complex patients.1 Although previous clinical trials have demonstrated that baricitinib is an effective treatment for patients with active RA who are also receiving background methotrexate, a new analysis digs deeper into the data.
Baricitinib is a once-daily oral Janus kinase 1 (JAK1)/JAK2 inhibitor in development to treat patients with moderate to severe rheumatoid arthritis (RA). Because many patients who suffer from chronic inflammatory rheumatic diseases may also have comorbidities, physicians have asked whether baricitinib is an effective treatment in these complex patients.1 Although previous clinical trials have demonstrated that baricitinib is an effective treatment for patients with active RA who are also receiving background methotrexate, a new analysis digs deeper into the data.
Arthur F. Kavanaugh, MD, professor of medicine at the University of California, San Diego, School of Medicine, presented the results of a post hoc analysis of two completed Phase 3 studies at the 2016 ACR/ARHP Annual Meeting in Washington, D.C.2 The research team sought to determine if previous failure of conventional disease-modifying anti-rheumatic drugs (cDMARDs) predicted an altered response to baricitinib in patients with RA. They also evaluated the effect of concomitant use of steroids and prognostically unfavorable factors on the efficacy of baricitinib.
Patients were randomized to receive placebo or baricitinib. Of the patients who received placebo, 40% had previously used methotrexate alone, 34% had used methotrexate and one cDMARD and 23% had used methotrexate plus two or more DMARDs. Of the patients who received 4 mg baricitinib, 46% had previously used methotrexate alone, 29% had used methotrexate plus one cDMARD and 23% had used methotrexate plus two or more DMARDs. At baseline, approximately half of the patients were using oral corticosteroids, and patients continued to use oral corticosteroids throughout the study.
The majority of each group (treatment or placebo) had two or three prognostically unfavorable factors. Nevertheless, 4 mg baricitinib was more effective than placebo. Specifically, the percentage of patients with a change from baseline in their van der Heijde modified Total Sharp Score (mTSS) of less than or equal to zero at 24 weeks was similar regardless of the other factors: number of cDMARDs previously used, concomitant use of corticosteroids or the presence of prognostically unfavorable factors.
Additionally, the rates of serious adverse events and discontinuation due to adverse events were comparable regardless of the other factors studied. Thus, baricitinib appears to be an effective treatment for patients who have a wide range of serologic status and baseline disease activity. In particular, baricitinib was effective in patients who had exposure to cDMARDs and corticosteroids.
If approved, baricitinib would join the oral JAK inhibitor tofacitinib as a treatment for RA.3 Research has documented that tofacitinib given either 5 or 10 mg doses twice a day as monotherapy is superior to methotrexate monotherapy. This result was true whether the patients had early or established RA. That said, patients with early RA appeared to respond better at 24 months than did patients with established RA. There were no differences in the safety profiles for tofacitinib between patients with early or established RA.