Articular cartilage defects are common, being encountered in more than half of all knee arthroscopies.1 While not all defects are symptomatic, those that are can cause disability comparable to that seen in patients awaiting knee replacement for advanced osteoarthritis.2 Early attempts at cartilage repair tended to focus on the defect itself, often disregarding articular comorbidities, such as malalignment or meniscal deficiency that were the root cause for the development of cartilage damage in the first place. Not surprisingly, early reports of cartilage repair were disappointing; for example, Brittberg reported good outcomes in only two of seven patients with autologous chondrocyte implantation (ACI) to the patella.3 In contrast to these disappointing early results, more recent studies have shown success in more than 70% of patients treated with patellar ACI.4-6 This substantial improvement has been attributed to the increased recognition and treatment of articular comorbidities concurrently with cartilage repair in a process termed biologic joint reconstruction. While many of the surgical procedures involved are technically challenging, there is wide consensus that the most challenging aspect of this field remains in correctly identifying the appropriate surgery for each patient’s problem.
Rationale for Biologic Joint Reconstruction
Knee replacement provides good pain relief with a relatively high patient satisfaction, ranging from 73% to 85%.7,8 Joint registries and large cohorts have demonstrated 10-year survival rates of 80% to 90% for total knee replacements.9,10 However, the majority of these studies were conducted in older patients, ranging in age from the late 60s to early 80s. Younger patients are less satisfied with the outcome and also demonstrate higher implant failure rates, with a three-year revision rate of 3% reported in patients younger than 55; only 50% of patients younger than 40 demonstrated either good or excellent Knee Society function scores following a total knee replacement, and the revision rate was 12.5% at eight years.11-13 These young patients will likely require multiple revision surgeries during their lifetime and these procedures result in progressively compromised outcomes.14,15 It therefore appears reasonable to attempt delaying arthroplasty as long as possible in young patients through early intervention to normalize the biomechanical environment and repair cartilage defects that have already developed.
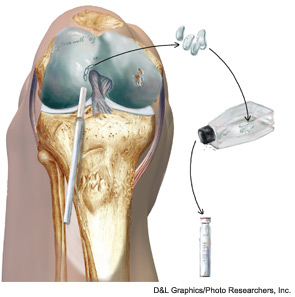
Diagnosis of Cartilage Defects
Symptomatic cartilage defects typically present with activity-related joint pain referable to the respective compartment (medial, lateral, or patellofemoral). Diffuse pain of the entire joint is atypical and should raise concerns for either more advanced tricompartmental osteoarthritis or other processes not generally amenable to cartilage repair. Swelling and effusion are seen especially with trochlear defects. Clicking and popping is a common, nonspecific joint complaint even in structurally sound knees, but can be associated with larger defects.


