A lot of effort goes into recruiting the best provider into a practice, but missteps during the onboarding process have the potential to leave the provider feeling unsatisfied and the practice dealing with turnover. Although it is one more task to add to an already full plate of things to do at a practice, comprehensive onboarding should be taken seriously.
The hiring process is just the first step in retaining the providers the administrative staff work hard to recruit. Physician onboarding, the process of familiarizing and orienting providers to a new healthcare facility or practice and to the culture of the organization, comes next. Onboarding introduces new providers to the community, integrates them with the medical staff, helps them establish their practice and achieve a firm financial foundation in the first year. While onboarding may sound simply like a nice thing to do, it is more than just a new-hire orientation. The process has an impact on the practice’s bottom line. Effective onboarding also helps reduce turnover and decreases recruitment and training costs.
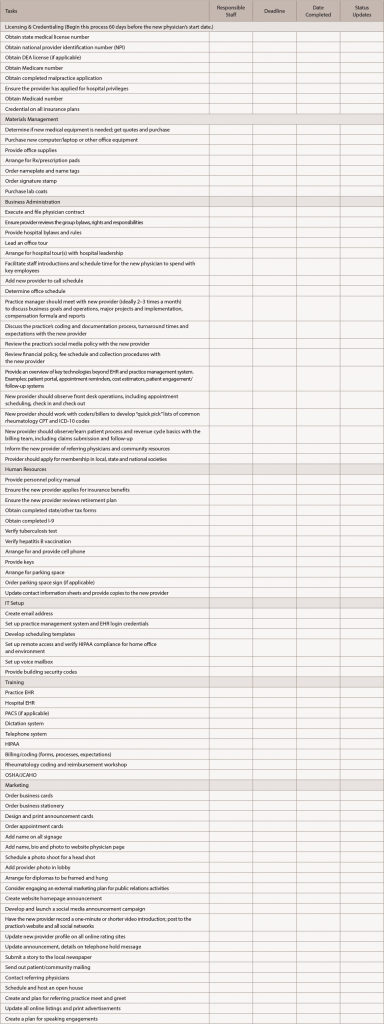
Onboarding should address credentialing, orientation, marketing and staff integration. If possible, make tedious paperwork available on an online portal so physicians can access these items separate from orientation and complete forms after the formal orientation.
6 Steps for a Smooth Orientation
- Prepare for due diligence: Create a checklist of items typically required for due diligence, such as bylaws, credentialing, contract review, insurance documentation, financial documents, employee roster and regulatory compliance documents.
- Develop a master onboarding list with a timeline and post it on your intranet or other central location: Identify responsible staff for each section and tie together sequential processes. Provide central access to the list so each department can access it as needed.
- Communicate: Communication and coordination are key to ensuring all items are completed prior to the provider beginning employment. Missing key deadlines can be costly to the organization. Set a realistic timeline: 60–90 days.
- Appoint a project manager/owner: The project manager/owner serves as the key contact for administrators and practitioners to ensure the process goes smoothly and remains on schedule. Regularly scheduled meetings with key staff help keep the process moving and holds people accountable.
- Establish an orientation plan: During the first year of employment, assign a physician mentor and hold regular meetings with the administrator or manager to ensure engagement and integration into the new group and culture.
- Continually review the process: Create a physician survey related to the onboarding process as part of the master plan to help identify potential areas for improvement.
Additionally, your practice should have a plan that measures and addresses the patient’s experience and ease with new provider(s)—and vice versa. Recruiting new providers usually requires a practice to assist with new patient recruitment and retention, so it is important to track the patient experience.
A sound onboarding process usually spans one to two years and includes communication, feedback and performance measurement—all keys to employee longevity and loyalty. A well-planned onboarding process that serves as a structural compass before, during and after hiring is critical to success. With a plan in place, the organization benefits through improved employee morale and a vibrant culture that ensures success in serving patient needs.