August is Psoriasis Action Month. Throughout the month, the National Psoriasis Foundation (NPF) is sharing resources for treating and managing psoriatic disease to empower patients to take control of their health. Formerly called Psoriasis Awareness Month, this year’s name change is more than symbolic. Mike Siegel, PhD, vice president of research for the NPF, sees the change as a chance to urge rheumatologists, dermatologists and other physicians to aggressively treat psoriasis and psoriatic arthritis.
August is Psoriasis Action Month. Throughout the month, the National Psoriasis Foundation (NPF) is sharing resources for treating and managing psoriatic disease to empower patients to take control of their health. Formerly called Psoriasis Awareness Month, this year’s name change is more than symbolic. Mike Siegel, PhD, vice president of research for the NPF, sees the change as a chance to urge rheumatologists, dermatologists and other physicians to aggressively treat psoriasis and psoriatic arthritis.
“People really aren’t aware [of the disease]—even if their friends or loved ones live with psoriatic disease. So making people aware is one thing,” Dr. Siegel says. “The next level is to help people take action around their disease. So get involved. Take control of your situation. Be confident in [speaking] to your healthcare provider, and get the level of treatment you want and you’re comfortable with.”
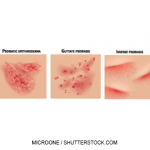
Given the statistics, action is necessary. Some 7.5 million people have psoriasis, according to the American Academy of Dermatology.1 And about 15% of people with psoriasis—more than 1 million people—develop psoriatic arthritis, according to the American College of Rheumatology.2
Treat to Target
A major highlight of this year’s action month is to promote treat to target, a strategy the NPF launched in late 2016 to enable providers and patients to set specific targets or goals to improve their health outcomes. The campaign debuted in November 2016 with the online publication of “From the Medical Board of the National Psoriasis Foundation: Treatment Targets for Plaque Psoriasis” in the Journal of the American Academy of Dermatology. The article’s objective was to reduce the “severity of plaque psoriasis so that it covers 1% or less of a person’s body within three months after starting a treatment,” according to the NPF website.3
“If that level of [skin] clearance has not been achieved, then it’s acceptable to be at either 3% BSA [body surface area] or less, or having seen a 75% improvement from your original disease severity,” Dr. Siegel says. “And then at six months after the start of treatment, the patient should expect to be at a BSA of 1% or less from there on.”
Dr. Siegel adds, “We’re really helping provide a framework for patients to say, ‘This is a goal that I can strive for,’ [encouraging them] not to be complacent or comfortable with whatever it is they may be used to.” If the patient has had skin severity for a long time, they may think it’s just the way it is. “We want to help communicate that patients can set more aggressive treatment goals.”
That advice holds true for rheumatologists, because many patients with rheumatic diseases also suffer from skin diseases. In fact, Dr. Siegel says the treat-to-target approach is based on a similar strategy taken for psoriatic arthritis and championed by Laura Coates, MBChB, MRCP, PhD, of Britain’s National Institute for Health Research.4
“A rheumatologist [may not be] an expert in treating skin disease, but knowing that there is something out there, I think, can really help [the rheumatologist] interact with patients with psoriatic arthritis who are more often than not suffering from skin symptoms, as well,” Dr. Siegel says. “Maybe if you’re not reaching the different levels of skin clearance while managing your joint disease, [patients] should be changing the dialogue with [their] dermatologist, thinking about different things. This [strategy] is about bringing [all those aspects] into the conversation so every contact point for that patient in the healthcare system will, hopefully, be helping them work toward those treatment targets.”
The advice is particularly helpful for rheumatologists, because the nexus of psoriasis and psoriatic arthritis is one they commonly deal with. Dr. Siegel says that many rural rheumatologists, in addition to their day jobs, are treating patients with dermatologic issues and the new BSA guidelines can be a needed push to more aggressively treat patients.
“If a patient has access to only one healthcare provider,” Dr. Siegel adds, “there are some really serious limitations for them to go and see the appropriate specialist. We hope, whoever they’re seeing, can be best equipped to help that patient.”
Richard Quinn is a freelance writer in New Jersey.
Reference
- American Academy of Dermatology. Conditions: Psoriasis. 2017
- American College of Rheumatology. Diseases and conditions: Psoriatic arthritis. 2017
- Armstrong AW, Siegel MP, Bagel J, et al. From the medical board of the National Psoriasis Foundation: Treatment targets for plaque psoriasis. J Am Acad Dermatol. 2017 Feb;76(2):290–298. doi: 10.1016/j.jaad.2016.10.017. Epub 2016 Nov 28.
- Coates LC, Helliwell PS. Treating to target in psoriatic arthritis: How to implement in clinical practice. Ann Rheum Dis. 2016 Apr;75(4):640–643. doi: 10.1136/annrheumdis-2015-208617. Epub 2015 Dec 15.