Two prospective studies have shown an association between baseline CRP levels and the subsequent development of erosions by MRI. However, the relationship between CRP and RP is also inconsistent. In one TNF inhibitor (TNFi) trial, CRP was predictive of RP developing in the methotrexate (MTX) plus placebo (PBO) group, but not in the group receiving MTX plus the TNFi.
RF has long been considered predictive of poor outcome. RF has also been used to select patients more likely to respond to rituximab (RTX). However, in one study, the average reduction in DAS28 for the seropositive patients was only 0.35 units greater than in the seropositive patients, a modest increase in benefit.
There is a strong association between ACPA and joint damage. In a 2008 study, the odds ratio for RP was 9.9 for high levels for ACPA, compared to only 2.6 for low/moderate levels. However, this is not consistent across all studies, and it has been estimated that ACPA and other current variables contribute only 32% to the prediction of radiographic progression.
The Path to Better Biomarkers
There is general agreement that we need better markers, and there have been many approaches to try to accomplish this. A Multi-Biomarker Disease Activity (MBDA) Score has been developed, starting with almost 400 candidate biomarkers identified by literature review and database screening. One hundred and thirty of these were assayed to identify association with the DAS28CRP and other measures of disease activity and condensed to 25 with the most consistent and strongest association with the DAS28CRP. These were prioritized into the final 12 biomarker algorithm, which is commercially available as Vectra DA from Crescendo Bioscience.
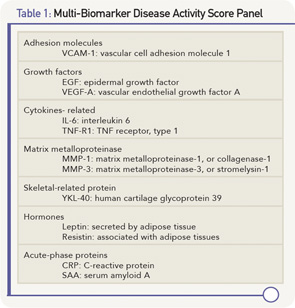
The 12 biomarkers in the MBDA represent multiple pathways that are functionally diverse (see Table 1, above), including cytokines, acute-phase reactant, matrix metalloproteinases (MMP), hormones, growth factors and an adhesion molecule.
The calculation of the MBDA score involves a formula based on the calculation of the DAS28DA, in which the various components are used to predict the tender and swollen joint counts, and the patient global assessment (see Figure 1). The score is rounded up to the nearest integer on a scale of 0–100. A low score is less than or equal to 29, moderate is 30–44, and high is >44.
Data from the SWEFOT (Swedish Farmacotherapy) trial was analyzed to help assess the clinical usefulness of the MBDA score. SWEFOT enrolled DMARD-naive RA patients with less than one year of symptoms and a DAS28CRP of >3.2. All patients received MTX monotherapy for three to four months, after which they were randomized into two groups. Group A received “triple” therapy with sulfasalazine and hydroxychloroquine added to the MTX; whereas group B added infliximab to the MTX. Each group was followed for a total of 24 months. Attainment of a EULAR “Good” response was no different between the groups: 38% for triple therapy vs. 31% for the infliximab group (p=0.204). However, there was a significant difference in RP, with a mean increase in the van der Heijde modification of the Sharp score of 7.23 in the triple therapy group vs. 4.00 in the infliximab group (p=0.009).