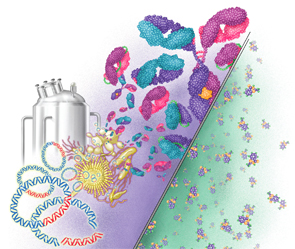
This illustration depicts the differences between biosimilars and chemically constructed small molecule drugs. Biosimilars are much bigger and more complex than small-molecule drugs.
DNA Illustrations/ScienceSource.com
Soon, biosimilars will be available as treatment options for our patients. Biosimilars are being introduced to the U.S. market in the hope that they will spur competition and drive down the price of these expensive medicines. Previous articles in The Rheumatologist have touched on various issues surrounding these new therapies, and everyone in the rheumatology community has questions about how they will fit into our armamentarium moving forward.
The Biologics Price Competition and Innovation Act of 2009 established an expedited approval pathway for biosimilars and paved the way for pharmaceutical companies to invest in and develop these agents. This past year, the FDA approved the U.S.’s first biosimilar product, filgrastim-sndz (Zarxio). On Feb. 9, 2016, the FDA’s Arthritis Advisory Committee recommended approval of an infliximab biosimilar, and on April 5, 2016, infliximab-dyyb (Inflectra) was approved for seven indications in the U.S.
First and foremost, be assured that the College is taking a strong, proactive approach to issues surrounding biosimilars. Several ACR committees are making biosimilars a top priority in 2016. The committees on Rheumatologic Care, Government Affairs and Corporate Relations, as well as the Affiliate Society Council and the Insurance Subcommittee, are regularly exchanging ideas and formulating action steps to protect clinicians and our patients as biosimilars become available. Rheumatologists are all too aware of the rising costs of prescription drugs and the struggles that we and our patients face to secure coverage from payers. Providing affordable therapeutic options is an essential part of Advancing Rheumatology! However, the ACR feels strongly that patient safety and patient and provider choice must drive upcoming decisions that the FDA will make. The ACR’s position paper on biosimilars was just updated in February.
Angus Worthing, MD, a rheumatologist in Washington, D.C., and a member of our Government Affairs Committee, shared the ACR’s position on regulatory aspects of biosimilars at the Feb. 9 FDA Arthritis Advisory Committee meeting and at a Dec. 18, 2015, Public Meeting on the Reauthorization of the Biosimilar User Fee Act (BsUFA). The ACR:
- Supports the Reauthorization of the Biosimilar User Fee Act (BsUFA);
- Holds that biosimilars must have distinct names, allowing them to be distinguished from each other and their reference products;
- Asserts that packaging language must a) indicate whether a biosimilar is interchangeable with the reference (originator) biologic, b) state all indications for which a biosimilar is approved and c) specify whether the supporting clinical data for the indication are derived from studies of the biosimilar or the reference product;
- Supports a requirement for clinical data to ensure biosimilars’ safety and efficacy prior to approval, not just extrapolation of data derived from studies of the reference biologic; and
- Supports a requirement that long-term, post-marketing studies of approved therapies be conducted to monitor for adverse events.
Several unanswered questions about biosimilars continue to be debated by the FDA and other stakeholders. In the coming weeks, we may know more about how prescribers will be notified when their prescriptions are filled by the pharmacy, what role payers will play in deciding drug substitutions and how biosimilars will be tracked for post-market efficacy and safety. That’s why the ACR must take an active role in driving this discussion. We want our voices to be heard, and we want to advocate for positions that will be beneficial for you and your patients. Now is the time for rheumatologists to speak up and speak out about biosimilars.
Here’s a brief look at some of the major discussions happening now:
Naming: The ACR’s position is that distinguishable, non-proprietary names for biosimilars, rather than generic names, will help ensure correct prescribing and dispensing of these drugs. We think distinct names will improve post-marketing monitoring for safety and efficacy, increase prescriber and patient confidence, and enhance market uptake. We expect the FDA to release its naming methodology standards shortly. If they stick with using distinct names, it may help enable them to make enforceable, science-based assessments of biosimilars, including extrapolation and interchangeability.
Labeling & Extrapolation: The ACR supports clear product labeling that indicates whether a biosimilar is interchangeable with its reference biologic. We feel that labeling should list all of the biosimilar’s approved indications and specify whether supporting clinical data were derived from studies of this biosimilar or its reference drug. The FDA released on March 31 draft guidance for industry that incorporates this recommendation. We’ve advised the FDA to use caution when approving extrapolation of biosimilars for indications that were already approved for the reference biologic. Why? Because there would be no safety data specific to that biosimilar and patient population.
One example illustrating this very real patient risk relates to biosimilars for erythropoietin. There are a few brands of erythropoietin on the market globally. In at least one instance, even though the biosimilar product and the reference product had similar therapeutic efficacy, one product had a different toxicity. Some people given the biosimilar developed immunity to the erythropoietin, which caused them to develop immunity to their own erythropoietin. This demonstrates how a biosimilar product that otherwise had characteristics that were identical to those of the reference product, had different toxicities. This immunogenicity development likely occurs in the highly complex manufacturing process that uses active cell lines. Such variations present a challenge in developing biosimilars, and are one concern with using them.1
Interchangeability: Although no manufacturer has yet applied for an interchangeable designation for a biosimilar, it will happen in the future. Interchangeables must meet higher standards of similarity to the reference biologic, and if so, they can be substituted by the pharmacy with no notification or prior approval from the prescriber. The regulatory criteria for interchangeability are still being developed, and the FDA has suggested that it will provide more information and clearer guidance on this issue in 2016. Many states have already passed laws to limit substitution at the pharmacy without prescriber notification. Obviously, this issue is of critical importance to rheumatology providers.
Education: The ACR will take an active role in helping the FDA educate stakeholders about biosimilars. We will work with other specialty groups, industry, pharmacy associations and other stakeholders to guide long-term, post-marketing assessments of biosimilars. We will share our experience and viewpoints to help shape new policies.
As biosimilars become part of our treatment plans, rheumatologists and rheumatology health professionals should be proactive in tracking them for safety and efficacy through clinical trials or registries. I know you must have many questions about biosimilars, and your patients may be coming to you with questions of their own. Check for updates. Get involved with the ACR’s advocacy efforts, including in your own state. If you haven’t been involved in the ACR’s advocacy efforts before, now is a great time to start. Contact the ACR.
 Joan M. Von Feldt, MD, MSEd, FACR, FACP, is president of the ACR and a professor of medicine at the Perelman School of Medicine at the University of Pennsylvania. She is also staff physician at the Philadelphia VA Medical Center.
Joan M. Von Feldt, MD, MSEd, FACR, FACP, is president of the ACR and a professor of medicine at the Perelman School of Medicine at the University of Pennsylvania. She is also staff physician at the Philadelphia VA Medical Center.
Reference
- Covic A, Abraham I. State-of-the-art biosimilar erythropoietins in the management of renal anemia: Lessons learned from Europe and implications for US nephrologists. Int Urol Nephrol. 2015 Sep;47(9):1529–1539.



