Recently, there have been reports of osteonecrosis of the jaw (ONJ) associated with bisphosphonate use—especially intravenous bisphosphonates and in patients with metastatic cancer. ONJ is an area of exposed bone in either the mandible or the maxilla that is slow to heal over a number of months. A few epidemiologic studies have identified factors for this condition that include a history of periodontitis, dental surgery, underlying malignancy, greater than one and a half years of intravenous bisphosphonate use, and poor dental hygiene.
While ONJ is a rare complication, encourage patients treated with bisphosphonates to have a dental examination before initiating a bisphosponate and at regular intervals.5 Because bisphosphonates have a long half-life in bone, there are no data to support discontinuation of the medication prior to a dental procedure to reduce the risk of ONJ.
Therapies: Anabolic Agents
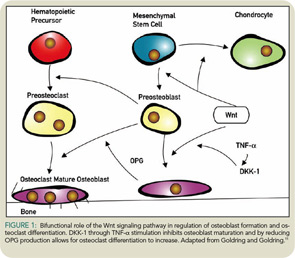
Teriparatide (PTH), which is approved for the treatment of osteoporosis, differs from the anti-resorptive agents in its actions. PTH is an anabolic agent that stimulates osteoblasts to form new bone while simultaneously increasing osteoclastic bone resorption through increasing receptor activator for nuclear factor k B ligand factor (RANKL) production. While bone turnover is increased with PTH, overall bone mass and bone strength increase with this agent, reducing fracture risk. While PTH is approved for the treatment of osteoporosis, it is generally not used as a first-line agent because of cost and the need for injections.
Initially, clinicians questioned whether combined treatment with an anti-resorptive agent and PTH could increase bone mass faster than treatment with the anabolic agent alone by blocking bone remodeling. Black et al. determined that concurrent treatment with PTH and alendronate was not more effective than PTH alone.6 PTH stimulates new bone formation and, by increasing the production of RANKL, also bone remodeling. Increased bone remodeling releases growth factors stored in the bone matrix to further stimulate new bone formation. Bisphosphonates block the bone remodeling and release of growth factors stored in the bone matrix. However, treatment with PTH should be followed by a bisphosphonate; this allows the remodeling space to fill in and fully mineralize. Patients who do not initiate anti-resorptive treatment after a one and a half- to two-year course of PTH will slowly lose the new bone mass gained.7

