You may say the 30 million Americans with osteoarthritis (OA) are walking around with a Band-aid—or so it seems.1 That’s because there’s no actual cure for this disabling condition. However, an international group of scientists is making headway on a method of eliminating aging—senescent—cells as a way to prevent or even reverse OA.
Cartilage Disappears, Senescent Cells Remain
In OA, joint cartilage is worn down. What hangs around, however, are these cells that can no longer divide. They accumulate and, researchers say, can cause trouble.
Jennifer H. Elisseeff, PhD, director of the Translational Tissue Engineering Center and Morton Goldberg Professor of Ophthalmology and Biomedical Engineering at the Johns Hopkins Wilmer Eye Institute, was co-author of a recent study, “Local clearance of senescent cells attenuates the development of post-traumatic osteoarthritis and creates a pro-regenerative environment,” published in Nature Medicine.2
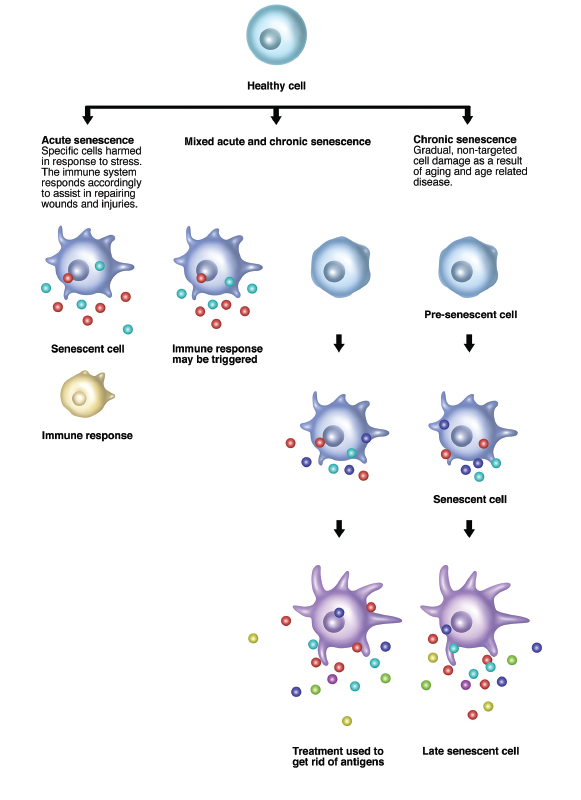
Dr. Elisseeff says, “Senescent cells produce SASP [senescence-associated secretory phenotype], which is made up of 100 or more molecules that include cytokines and extracellular-matrix-modifying enzymes—essentially the things we often see in inflammatory disease. The senescent cells are calling immune cells to help with repair. However, if something goes wrong, like in cartilage tissue, you get a pro-inflammatory immune response that can be problematic.”
Detailing the history of this work, Dr. Elisseeff states, “My colleagues and I initially approached cartilage repair from the orthopedic-surgery side, looking at building biomaterials to augment microfracture. But it became clear that we needed to address issues of inflammation in the local environment. We had already taken note of the fact that the literature contained information on an association between senescent cells and arthritis in patients undergoing total knee arthroplasty. Soon after, we were approached by San Francisco-based Unity Biotechnology with the idea of looking at senescent cells in cartilage.”
Gwen Shockey / Science Source
Promising New Drug
“For this study,” notes Dr. Elisseeff, “we performed surgery on mice in order to mimic joint injury. Our ultimate goal was a therapeutic agent … molecules that could be used as drugs to clear these cells in a selective fashion. Postoperatively, we injected the mice with a drug named UBX0101, a molecule that had already been shown to eradicate senescent cells in the lab. This drug, co-developed by Unity Biotechnology, resulted in a 50% elimination of senescent cells. An unexpected clinical bonus was that it led to new cartilage formation.”
To see what this might mean for humans, Dr. Elisseeff and colleagues tested UBX0101 in human knee tissue of individuals afflicted with severe OA. “The cells were exposed to this molecule for four days; we were pleased to find a major reduction in the number of senescent cells. The most compelling finding was that when we removed these cells, even patients with quite advanced OA benefitted.”
Jamie Dananberg, MD, is chief medical officer at Unity Biotechnology. He states, “Unity Biotechnology became interested in senescent cells nearly six years ago when one of our co-founders did some work in this area. When we were looking to further our work on senescent cells and arthritis, we reached out to Dr. Elisseeff.
“We knew it was critical to examine the biology underlying OA,” states Dr. Dananberg. “This condition is recognized as inflammatory, but no one understands exactly why inflammation is involved. We found that in the culture system from the human knee cartilage if you eliminate senescent cells then the remaining chondroyctes can produce type II collagen and aggrecan (the ingredients of cartilage). In an environment where you have the interplay of roughly 100 inflammatory molecules, if you remove just one or two it will have little impact. A better idea is to eliminate the actual senescent cells so you get rid of the underlying cause of OA.
“In the Nature study published in early 2016, a culmination of our prior work, it was interesting to see that one of the significant phenotypes we identified was musculoskeletal.3 The animals involved actually had greater muscle mass, tensile strength and an absence of OA. The Nature Medicine work picked up from that and extended it to better understand OA.”
Throw Out the Dogma
“Thus far, we have only been able to offer patients symptom relief with medications, such as steroids and non-steroidal anti-inflammatory drugs. Something that has really struck us is that there is a lot of acquiescence in terms of standard of care. We are taught that bones are supposed to ache and creak—and that OA is just a part of getting old. Maybe it does not have to be like that … maybe it’s time to toss out the dogma. Our goal is to be working in the clinic with humans next year. The potential that we can intervene in the OA process is exceptional.”
Elizabeth Hofheinz, MPH, MEd, is a freelance medical editor and writer based in the Greater New Orleans area.
References
- Osteoarthritis. Centers for Disease Control and Prevention. 2017 Sep 9 (reviewed).
- Jeon OH, Kim C, Laberge RM, et al. Local clearance of senescent cells attenuates the development of post-traumatic osteoarthritis and creates a pro-regenerative environment. Nat Med. 2017 Jun;23(6):775–781.
- Baker, DJ, Childs BG, Durik M, et al. Naturally occurring p16(Ink4a)-positive cells shorten healthy lifespan. Nature. 2016 Feb 11;530(7589):184–189.
Note: The study was conducted by scientists at UNITY Biotechnology, Johns Hopkins University, Buck Institute for Aging Research, Lawrence Berkeley National Laboratory, Mayo Clinic College of Medicine, Ulsan National Institute of Science and Technology, and the European Research Institute for the Biology of Aging.

