About time / shutterstock.com
ATLANTA—The potential of cannabis‐based medicines is a hot topic, particularly as pain management therapy for arthritis and other conditions. However, confusion abounds regarding its therapeutic potential, how it can be administered and even the correct terminology to use.
David P. Finn, PhD, professor of pharmacology and therapeutics, and founding co-director of the Centre for Pain Research at the National University of Ireland, Galway, spoke at the 2019 ACR/ARP Annual Meeting in the session, Mechanisms of Cannabinoids in Pain Management. He discussed the potential for this controversial plant and its derivatives.
Although the cannabis plant has three species, Cannabis sativa is the one that has the most interest and potential medicinally, Dr. Finn pointed out.
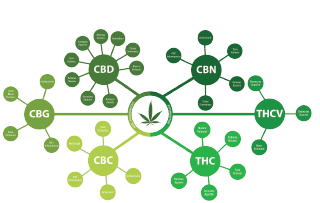
“When talking about cannabinoids, we’re talking about biologically active constituents of cannabis (phytocannabinoids) or synthetic compounds, usually having affinity for and activity at cannabinoid receptors,” said Dr. Finn. As many as 1,000 unique molecules are contained in the cannabis plant. To date, cannabis plants and plant material, including flowers, hashish, buds, leaves and full plant extracts, have been used for medical reasons.
Cannabis-based medicines also exist. These are registered as medicinal cannabis extracts with defined, standardized tetrahydrocannabinol (THC) and cannabidiol (CBD) content. These are classified as cannabis-derived or cannabis-based medicines. Examples: 1) nabiximols (Sativex), a cannabis-based pharmaceutical product containing delta 9-THC and CBD in a 1:1 ratio, delivered in an oromucosal (mouth) spray; it has been approved as adjunctive treatment for neuropathic pain in patients with multiple sclerosis; and 2) Epidiolex, an oral CBD solution used to treat seizures caused by two forms of epilepsy: Lennox-Gastaut syndrome and Dravet syndrome.1
Molecular Targets
Many years after THC was discovered, the molecular targets mediating its effects were identified—the cannabinoid receptors CB1 and CB2 and their endogenous ligands. The endocannabinoid system is the regulatory system in the body that controls the creation and breakdown of cannabinoids. It also plays a key role in mediating pain sensation, appetite, sleep and metabolism.

Dr. Finn
CB1 is associated with psychoactive, neuromodulating and analgesic effects due to the THC lipid. CB1 is ubiquitously distributed and expressed across the entire body, in the brain, adipocytes, hepatocytes and musculoskeletal tissues. “Based on studies, CB1 is the most highly expressed G-protein-coupled receptor in the brain,” said Dr. Finn.
CB2 is associated with anti-inflammatory and immunomodulatory effects but has no psychoactive effects. CB2 is expressed in body cells controlling immune function and, possibly, the central nervous system.
As described in the European Pain Federation (EFIC) position paper, Appropriate Use of Cannabis‐Based Medicines and Medical Cannabis for Chronic Pain Management, the lipid signaling system of the endocannabinoid system plays a very important role in the regulation of a wide array of physiological processes, including appetite, metabolism, mood, motor function, gastrointestinal tract function, cardiovascular control, stress response, developmental biology, cell fate, immune and inflammatory response, endocrine function, neurotransmission and pain.2
Efficacy Studies
Many studies have focused on the efficacy of cannabinoids in chronic pain, the most common condition cited by patients for the medical use of cannabis, according to Dr. Finn. A report released by Ireland’s Health Products Regulatory Authority in 2017 stated, “chronic pain is the most studied indication for cannabinoids.”3

Dr. Fitzcharles
One study found that plant-derived cannabinoids increased the odds for improvement of pain by about 40% vs. control.4 “Three additional scientific reviews of the evidence conclude there is good or substantial, high-quality evidence that medical cannabis or cannabinoids are at least moderately efficacious in chronic pain in adults, but others are less positive,” said Dr. Finn.5-8
Dr. Finn said future clinical studies “could assess the potential utility of endocannabinoids (and related lipids) as biomarkers for stress-induced exacerbation of chronic pain, and comorbidity of chronic pain with affective disorders, in addition to investigating whether mechanisms elucidated in rodents translate to human patients and might be modulated pharmacologically for therapeutic benefit.”9
Progress is being made. The European Pain Federation task force position paper provides “a fair, balanced and evidence-based summary of the role of cannabis-based medicines for use in pain management.”2 The task force concluded that therapy with cannabis-based medicines:
- Should be considered only by experienced clinicians as part of a multi-disciplinary treatment;
- Should be used as adjunctive medication if guideline-recommended first- and second-line therapies have not provided sufficient efficacy or tolerability;
- May be reasonably considered for chronic neuropathic pain; and
- Should be regarded as an individual therapeutic trial for all other chronic pain conditions (e.g., cancer, non-neuropathic non-cancer pain).
Realistic therapy goals have to be defined, and all patients must be kept under close clinical surveillance.
Treasure Chest or Pandora’s Box?
“The preclinical science is compelling,” said Mary-Ann Fitzcharles, MD, associate professor of medicine in the Division of Rheumatology at McGill University, Montreal, who also spoke at the session. “It shows excellent effect on acute and chronic pain—although some studies show low-strength evidence for neuropathic pain and a small effect on pain overall—and excellent effect on inflammation.” Low-quality evidence also shows cannabinoids are associated with improvements in nausea and vomiting from chemotherapy, and Tourette’s syndrome. It can also both positively and negatively affect anxiety and sleep, she noted.10
Dr. Fitzcharles co-authored a position statement by the Canadian Rheumatology Association.11 “Despite lack of evidence for use of medical cannabis in rheumatology patients, we acknowledge the need to provide empathetic and pragmatic guidance for patient care,” the statement concluded. “This position statement aims to facilitate the dialogue between patients and healthcare professionals in a mutually respectful manner to ensure harm reduction for patients and society.”
Dr. Fitzcharles said the statement recommended that people under 25 years old (because their brains are still developing), people with allergies, pregnant and breast-feeding women, and individuals with a history of psychosis, substance abuse, suicide ideation or attempts not use medical cannabis. “Caution is advised” for the elderly, those with unstable mental health, cardiovascular and pulmonary disease, and also those with prescriptions for sedative or psychoactive drugs. “I also caution those working in settings requiring concentration, executive function and alertness,” she said.12
Dr. Fitzcharles advised against using inhalation products. “Oral consumption is preferred. Also, only use medical cannabis from a licensed producer with known molecular content. Lower THC and higher CBD content is preferable.”13
Mike Fillon is a healthcare writer living in the Atlanta area.
References
- Starowicz K, Finn DP. Cannabinoids and pain: Sites and mechanisms of action. Adv Pharmacol. 2017;80:437–475.
- Häuser W, Finn DP, Kalso E, et al. European Pain Federation (EFIC) position paper on appropriate use of cannabis-based medicines and medical cannabis for chronic pain management. Eur J Pain. 2018 Oct:22(9):1547–1564.
- Cannabis for medical use—A scientific review. Health Products Regulatory Authority. 2017 Jan 31.
- Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015 Jun 23–30;313(24):2456–2473.
- Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: A clinical review. JAMA. 2015 Jun 23–30;313(24): 2474–2483.
- World Health Organization. The health and social effects of nonmedical cannabis use. 2016.
- National Academies of Sciences, Engineering, and Medicine. The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research. Washington, D.C.: The National Academies Press; 2017.
- Nugent SM, Morasco BJ, O’Neil ME. The effects of cannabis among adults with chronic pain and an overview of general harms: A systematic review. Ann Intern Med. 2017 Sep 5;167(5):319–331.
- Woodhams SG, Chapman V, Finn DP, et al. The cannabinoid system and pain. Neuropharmacology. 2017 Sep 15;124:105–120.
- Andre CM, Hausman JF Guerriero G. Cannabis sativa: The plant of the thousand and one molecules. Front Plant Sci. 2016;7:19.
- Fitzcharles MA, Niaki OZ, Hauser W, et al. Position statement: A pragmatic approach for medical cannabis and patients with rheumatic diseases. J Rheumatol. 2019 May;46(5):532–538.
- Minerbi A, Häuser W, Fitzcharles MA. Medical cannabis for older patients. Drugs Aging. 2019 Jan;36(1):39–51.
- Hazekamp, A. The trouble with CBD oil. Med Cannabis Cannabinoids. 2018;1:65–72.



