Lightspring / shutterstock.com
SNOWMASS VILLAGE, COLO.—Even in the era of treat to target, cardiovascular disease risk remains elevated and is a major source of mortality and morbidity in patients with rheumatoid arthritis (RA). Screening and management of cardiovascular risk in these patients is critical to ensure these patients are identified and treated.
At the 2019 ACR Winter Rheumatology Symposium, Jon T. Giles, MD, MPH, associate professor of medicine, Division of Rheumatology, Vagelos College of Physicians and Surgeons, Columbia University, New York, addressed this concern. He said, RA “patients at risk for cardiovascular disease events may not be obvious because their traditional cardiovascular risk profile, based on cholesterol, hypertension and diabetes, may not indicate risk.”
Dr. Giles spoke on the pathogenesis of cardiovascular risk in RA patients, emphasizing the relationship between traditional risk factors, such as fasting lipids and atherosclerosis, is different in patients with RA.
EULAR Guidelines
The need for rheumatologists to recognize this increased, often not obvious, cardiovascular risk in RA patients is recognized by the current EULAR guidelines, which recommend rheumatologists take responsibility for the assessment and management of cardiovascular disease in RA patients.1
According to Dr. Giles, most rheumatologists have not yet taken this step. He thinks that if screening for and management of cardiovascular risk are the primary responsibility of rheumatologists, an evidence-based algorithm that is easy to follow and proven effective is needed.
Screening for Cardiovascular Risk

Dr. Giles
Citing the EULAR guideline for cardiovascular risk in RA patients, Dr. Giles highlighted the specific recommendations for cardiovascular screening every five years in RA patients.2
Current data show the need for improved screening in the U.S. Less than one-half of RA patients are regularly screened for hyperlipidemia, with specific populations less likely to be screened (i.e., older patients, those with fewer office visits and those with more comorbidities) and that screening by rheumatologists is low.3 Data also show standard risk stratification tools to screen for cardiovascular risk underperform when used to assess risk in RA patients.
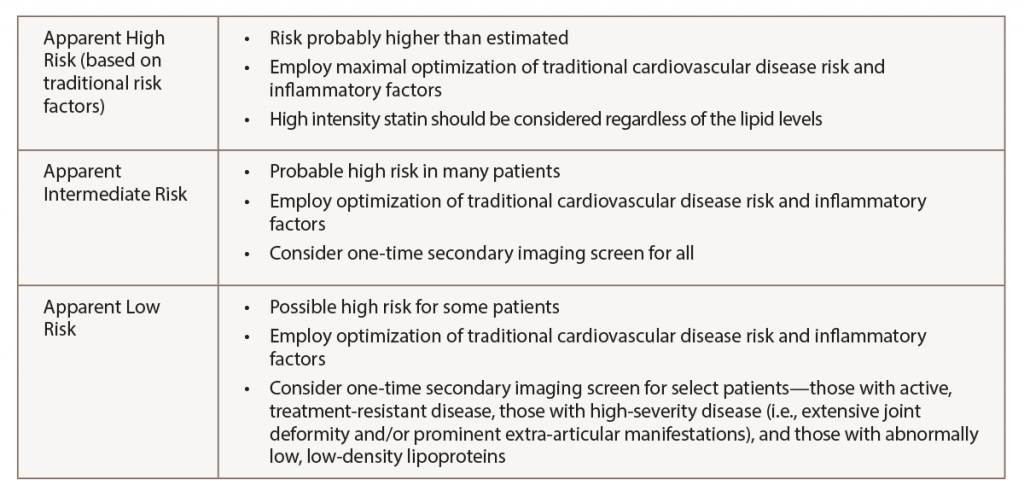
To help rheumatologists screen for cardiovascular risk in RA patients, Dr. Giles walked participants through a risk stratification approach he developed (see Table 1, below).4 He emphasized the strategy is not evidence based and needs to be formally evaluated to prove it is clinically effective and cost effective.
In patients for whom cardiovascular risk is uncertain (i.e., intermediate- and certain apparently low-risk patients), Dr. Giles cited data from the American College of Cardiology/American Heart Association guidelines that recommend computed tomography with determination of the coronary artery calcium score for these patients.5 “A coronary calcium score of zero is reassuring, even if the patient has higher traditional cardiovascular risk,” he said. “In addition, patients with high calcium scores are likely to benefit from statin therapy even if their circulating lipid levels are low.”
Although many insurance plans may not cover this test, he expects it will be fully covered in the near future given its recommendation in the guidelines. “Even if not covered,” he said, the out-of-pocket costs are between $100 and $300 in most places, “so some people are getting them on their own.”
Standard risk stratification tools to screen for cardiovascular risk underperform when used to assess risk in rheumatoid arthritis patients.
Risk Management
Dr. Giles also reviewed some of the data on the most studied agents linked to a reduction in cardiovascular events in RA patients—methotrexate and tumor necrosis factor (TNF) inhibitors.
Evidence from eight cohort studies shows methotrexate was associated with a 28% reduction in all cardiovascular events. In addition, evidence from 16 cohort studies showed a 30% reduction in all cardiovascular events with TNF inhibitors.6 These data support the use of these agents as a strategy for reducing cardiovascular events, said Dr. Giles, emphasizing, however, this support is based only on observational data.
Few head-to-head comparisons between these agents have been conducted. Those that have been conducted have not shown any superiority of one agent over another.
Although other cytokine inhibitors may have similar effects to these agents, he said it is “imprudent to make assumptions.”
Dr. Giles pointed out that a recent trial of people without RA but with a history of cardiovascular disease, data showed methotrexate did not confer a benefit in reducing cardiovascular events. This result is generating some controversy. Dr. Giles emphasized the findings could have been affected by the fact the investigators did not select patients with elevated inflammation. “It [methotrexate] also may be better for primary rather than secondary prevention,” he said. “And effects may differ in RA compared with the general population.”
Mary Beth Nierengarten is a freelance medical journalist based in Minneapolis.
References
- Agca R, Heslinga SC, Rollefstad S, et al. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis. 2017 Jan;76(1):17–28.
- Bartels CM, Kind AJ, Everett C, et al. Low frequency of primary lipid screening among Medicare patients with rheumatoid arthritis. Arthritis Rheum. 2011 May;63(5):1221–1230.
- Giles JT. Cardiovascular disease in rheumatoid arthritis: Current perspectives on assessing and mitigating risk in clinical practice. Best Pract Res Clin Rheumatol. 2015 Aug–Dec;29(4–5):597–613.
- Goff Jr DC, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. J Am Coll Cardiol. 2014 Jun 24;129(Suppl 2):S49–S73.
- Roubille C, Richer V, Starnino T, et al. The effects of tumour necrosis factor inhibitors, methotrexate, non-steroidal anti-inflammatory drugs and corticosteroids on cardiovascular events in rheumatoid arthritis, psoriasis and psoriatic arthritis: A systematic review and meta-analysis. Ann Rheum Dis. 2015 Mar;74(3):480–489.