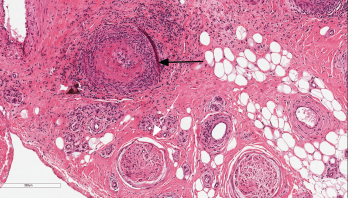
Figure 1: Nerve Biopsy
This image depicts the sural nerve biopsy with hematoxylin and eosin staining at 100x magnification. The black arrow indicates necrotizing vasculitis of epineural arterioles and muscular arteries with fibrinoid necrosis. The infiltrate is a mixture of neutrophils and mononuclear cells. There is luminal thrombosis with recannulation. Nerves (white arrow) show mildly thickened perineurium, but are relatively unaffected by inflammation.
Sural nerve and gastrocnemius biopsies were performed. Microscopic pathology showed a perineural, large arteriolar, necrotizing vasculitis consistent with PAN (see Figure 1).
We diagnosed vasculitic neuropathy and started our patient on monthly intravenous cyclophosphamide (500 mg/m2). After three months of treatment, he was not able to reduce his prednisone dose below 30 mg/day without worsening, painful dysesthesias in his feet and lower legs; additionally, his C-reactive protein remained elevated (5.8–8.9 mg/dL).
Another three months of intravenous cyclophosphamide at 750 mg/m2 was administered without improvement in his symptoms, C-reactive protein levels or prednisone requirement. Azathioprine was then tried, without any clinical benefit.
The previously fleeting leg rash became more persistent, and was joined by erythematous, reticulated macules on his arms and legs, and scattered purpuric papules. He also developed livedo racemosa, as well as slate-gray discoloration of the anterior lower legs, likely due to minocycline hyperpigmentation. A skin biopsy of an erythematous papule on his posterior left thigh demonstrated normal epidermis and superficial dermis with deep dermis and panniculus featuring intramural mixed inflammatory infiltrates of lymphocytes, histiocytes and neutrophils in medium and large vessels (see Figure 2). Direct immunofluorescence was negative for IgG, IgA, IgM and C3. The pathologic description was read as consistent with polyarteritis nodosa (PAN).
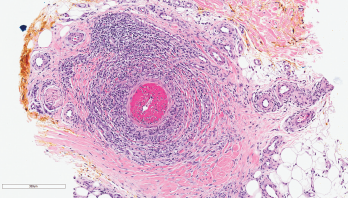
Figure 2: Skin Biopsy
This image depicts the left posterior thigh biopsy of the soft tissue with hematoxylin and eosin staining at 100x magnification and shows necrotizing vasculitis of a deep dermal muscular artery with fibrinoid necrosis. The infiltrate is predominantly neutrophilic, and there is marked thrombosis of the arterial lumen. Concurrent direct immunofluorescence studies were negative.
Minocycline was identified as a potential trigger for the patient’s vasculitis and was discontinued. Within 30 days after stopping the minocycline, his rash resolved, his pain significantly improved and his C-reactive protein normalized (0.3 mg/dL). He received no more cyclophosphamide. Azathioprine was stopped, and prednisone was successfully weaned to 5 mg/day within one month and was stopped entirely by six months. Although he experienced persistent dysesthesias in his feet, presumed to be from permanent nerve damage, all of his other symptoms stabilized. At his three-year follow-up, he had experienced no further rashes or arthralgias, and his C-reactive protein remained normal.

