Hair dye products are commonly used by both men and women to enhance youth and beauty and to follow fashion trends. As reported in the medical literature, hair dyes and their ingredients are associated with allergic contact dermatitis. A possible association with joint inflammation has also been recognized. There is literature to support that para-phenylenediamine or p-phenylenediamine (PPD), a component of many hair dyes, is proinflammatory and also associated with an increased risk of developing systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). This case illustrates the need to increase awareness about chemicals found in hair dyes and the possible links to inflammatory arthritis and other autoimmune diseases.
Hair dye products are commonly used by both men and women to enhance youth and beauty and to follow fashion trends. As reported in the medical literature, hair dyes and their ingredients are associated with allergic contact dermatitis. A possible association with joint inflammation has also been recognized. There is literature to support that para-phenylenediamine or p-phenylenediamine (PPD), a component of many hair dyes, is proinflammatory and also associated with an increased risk of developing systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). This case illustrates the need to increase awareness about chemicals found in hair dyes and the possible links to inflammatory arthritis and other autoimmune diseases.
Case Presentation
A 50-year-old white man, with a past medical history remarkable for asthma, allergic rhinitis and treated latent tuberculosis, described low back, hand and Achilles tendon pain he’d been experiencing for four months. The pain restricted his recreational activities, including playing guitar and running, but he did get some relief when he took naproxen.
He said he had not experienced psoriasis, skin rash, nail changes, diarrhea, uveitis, urethritis, joint swelling, fever, fatigue or weight loss. A review of systems was otherwise unremarkable.
His sister has a history of psoriatic arthritis.
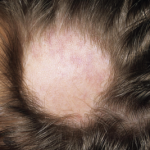
The physical exam revealed that he had swollen and tender second and third proximal interphalangeal joints and right third metatarsal joint on his right hand, as well as swelling and tenderness in the first interphalangeal and metacarpophalangeal joints on his left hand. He also had right elbow tenderness, with slightly reduced right elbow extension. The range of motion in the rest of his joints was normal. There was no evidence of a skin rash, dactylitis, enthesitis, nail pitting or sacroiliac joint pain.
Lab tests, including those for complete blood count, comprehensive metabolic panel, sedimentation rate, C-reactive protein, anti-CCP antibodies, hepatitis B and C, and QuantiFERON-TB gold were unremarkable. However, a rheumatoid factor test was positive at 22 IU/mL (normal: <14 IU/mL).
The patient was hesitant to start on disease-modifying anti-rheumatic drugs (DMARDs) for inflammatory joint pain due to the potential side effects. Thus, the rheumatologist chose to follow him closely to assess disease progression.
Eight months after the initial onset of his symptoms, the patient’s joint pain completely resolved, and he was able to get back to his routine recreational activities. He noticed a correlation between the onset of joint pains and the use of hair dye on his beard. He decided to stop using the hair dye and noticed the joint pain had resolved. He is now able to run and play his guitar.