When interviewing a patient with Behçet’s disease & new-onset headache, reports of morning headache, a positional component, worsening with Valsalva & refractoriness to therapy should prompt a cerebral venous sinus thrombi workup.
Neuro-Behçet Disease
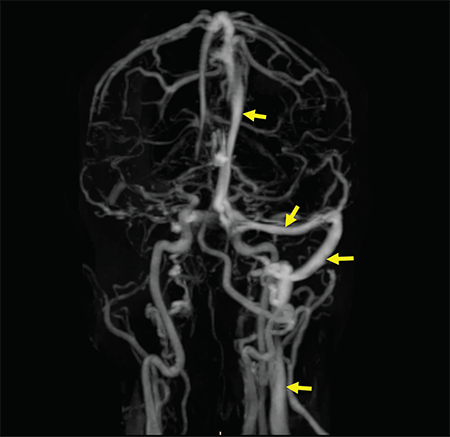
Figure 2: A contrast-enhanced MRV shows a filling defect in the right internal jugular vein, right sigmoid sinus, right transverse sinus and superior sagittal sinus. Normal enhancement of the respective structures is visualized on the left side (arrow).
As a multisystem inflammatory disease, Behçet’s disease can affect any organ or system in the body, including the nervous system. Neurological manifestations in Behçet’s disease are generally divided into parenchymal (intra-axial) and non-parenchymal (extra-axial). A diagnosis of neuro-Behçet disease is considered in patients who fulfill Behçet’s disease diagnostic criteria, do not have an alternative explanation for neurological symptoms and have supportive objective evidence of abnormal cerebrospinal fluid (CSF) analysis and/or abnormal MRI imaging.5
The most common presentation of parenchymal neuro-Behçet’s disease is a brainstem syndrome, which can present with ophthalmoparesis, dysarthria, weakness and ataxia. Headache is commonly reported in meningoencephalopathy. Less commonly, patients can present with cerebral hemisphere involvement, mass-like lesions on MRI, seizures and cognitive-behavioral changes.5,6
Non-parenchymal neuro-Behçet’s disease mainly involves CVST. CVST presents with signs of elevated intracranial pressure, namely headache, mental status changes, papilledema and cranial nerve VI palsy. CVST accounts for 10–20% of neuro-Behçet’s disease and is present in 5–6% of patients with Behçet’s disease.7 Although severity and progression of symptoms vary according to size and site of thrombosis, CVST usually presents in a subacute and progressive manner, rather than acute fulminant symptoms with rapid mental status change and seizures. CVST tends to occur earlier in the course of disease compared with parenchymal neuro-Behçet’s disease and occurs more commonly in males. Thrombosis can occur in any number of cerebral sinuses, but is most commonly reported in the superior sagittal and transverse sinus.
Headache in Behçet Disease
Headache is one of the most common symptoms in patients with Behçet’s disease, regardless of neurologic involvement. Prevalence of headache is reported between 44 and 80%. Depending on the population, the headaches are attributable to migraine or tension, rather than neuro-Behcet’s.7
In a cohort of more than 200 patients with Behçet’s disease and headaches, parenchymal and non-parenchymal neurologic involvement was seen in 5.2% and uveal inflammation was seen in 3.9% of the patients.5,6 However, in patients with confirmed neuro-Behçet’s disease, headache remains the most commonly reported presentation.
Determination of initial investigation and management of headache in Behçet’s disease patients relies heavily on obtaining a thorough history and neurological examination. Any reported complaint of headache warrants obtaining a detailed history that includes onset, duration, quality, and alleviating and exacerbating factors. Additionally, concurrent relapse of other features of Behçet’s disease, such as oral or genital ulceration, should heighten suspicion for neuro-Behçet’s disease in a patient presenting with headache. Missed and untreated CVST can lead to venous congestion, cerebral edema and, eventually, brain herniation and death.9