Introduction
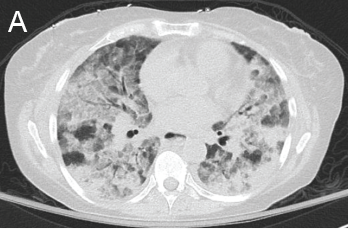
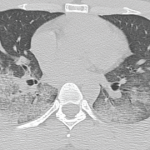
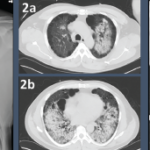
Figure 1: GPA radiographic progression
A novel coronavirus, designated SARS-CoV-2 by the World Health Organization, was identified at the end of 2019 after a large number of patients were diagnosed with pneumonia in Wuhan, China. The virus rapidly spread across the world, becoming a pandemic, with the first case in the U.S. reported on Jan. 20, 2020. The most common presenting symptoms include cough, fever, myalgia, dyspnea and pharyngitis. Presentation ranges from mild infection (~80%) to severe (~20%), in which patients experience respiratory failure. Severe illness predominantly occurs in adults of advanced age and in those with underlying medical conditions, but can also occur in otherwise healthy individuals.

A) Diffuse, patchy, bilateral groundglass opacities and interlobular septal thickening with small patches of dense pulmonary consolidation are seen.
B) Repeat CT after two doses of rituximab and steroids shows markedly improved groundglass opacities, resolved areas of consolidation and moderate residual subpleural interstitial lung disease.
Given the ongoing pandemic, the leading diagnosis considered for patients presenting to the hospital with respiratory symptoms is COVID-19. Often, bacterial and viral tests are run simultaneously, with most patients treated for bacterial pneumonia while awaiting results. The diagnosis of COVID-19 is made by direct detection of SARS-CoV-2 RNA by nucleic acid amplification tests (NAATs), most commonly reverse-transcription polymerase chain reaction (RT-PCR) from the upper respiratory tract.
The U.S. Food & Drug Administration has granted emergency use authorization for many different NAATs. The accuracy and predictive values of SARS-CoV-2 NAATs have not been systematically evaluated. Reported false negative rates have ranged from less than 5% to 40%, although these estimates are limited in part by the fact that no perfect reference standard for comparison exists. Given the high incidence of false negative tests, NAATs are often repeated if clinical suspicion for COVID-19 remains high. This has also led clinicians to rely on other diagnostic tools, such as chest imaging.
Here, we present a case of a previously healthy woman admitted with acute dyspnea on exertion, which raised suspicion for COVID-19 despite her first test being negative. CT imaging showed an impressive pattern of diffuse groundglass opacities with focal consolidations, which raised suspicion for a viral infectious etiology, specifically COVID-19. Because multiple bacterial and viral tests were negative, including three NAATs for SARS-CoV-2, and due to a lack of response to antibiotic treatment, other etiologies were considered.
The first concern was cryptogenic organizing pneumonia (COP) given her relatively acute presentation and CT findings. The other consideration was a potential autoimmune cause given her remote history of Raynaud’s. However, after evaluation by a rheumatologist, suspicion for autoimmune disease was lower, given the absence of other clinical features to suggest it. Nevertheless, serologic evaluation showed high titers of proteinase 3 (PR3) antibodies. The patient was, thus, diagnosed with GPA restricted to the lung based on isolated pulmonary manifestations, strongly positive serologies and response to high doses of steroids.
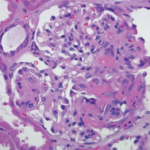
GPA is an uncommon disease characterized by a chronic granulomatous necrotizing vasculitis of mainly small- and medium-sized vessels. It affects three out of every 100,000 people in the U.S. The mean age at diagnosis is 50 years, and the majority (90%) of cases occur in the Caucasian population. GPA affects multiple organ systems and may involve any part of the body. It has a broad clinical spectrum, ranging from localized disease (predominantly restricted to the respiratory tract) to a severe life-threatening form with involvement of multiple organs (predominantly the kidneys and lungs). Patients typically present with weeks to months of constitutional symptoms and later develop signs or symptoms of specific organ involvement. Even though the majority of patients have an insidious course, some can have an explosive presentation over days, like our patient.
Serum cytoplasmic ANCA titer elevation occurs in 82–94% of GPA patients, depending on disease severity. It is primarily associated with anti-PR3, while microscopic polyangiitis is primarily associated with anti-myeloperoxidase (MPO). GPA antibody test results can take several days.
Clinical suspicion for this disease may be delayed in the current climate of a pandemic, especially if it occurs in the absence of other signs or symptoms to suggest an autoimmune etiology, such as in our patient, who presented with isolated pulmonary symptoms. Chest CTs can be readily available and provide some clues to help differentiate infectious from autoimmune etiologies, such as GPA. Here, we review the radiographic characteristic features of the three main diagnostic considerations in this patient: COVID-19 infection, GPA and COP.