CT Findings in COVID-19
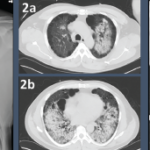
Multiple studies have been recently published describing CT characteristics of COVID-19 infection. All of them suggest the proportion of CT abnormalities in patients infected with COVID-19 is very high. The most typical CT imaging finding is the presence of groundglass opacities, with more than half of the patients having some combination of groundglass opacities, consolidation and adjacent pleural thickening.
A meta-analysis of 13 studies with a total of 2,738 participants reported a pooled positive rate of CT imaging of 89.76% (95% CI 84.42–93.84%). The typical CT imaging appearance for COVID-19 was groundglass opacities (83.31%), groundglass opacities with mixed consolidation (58.42%), adjacent pleural thickening (52.46%), interlobular septal thickening (48.46%) and air bronchograms (46.46%). Other, less common CT signs included crazy paving pattern (14.81%), pleural effusion (5.88%), bronchiectasis (5.42%), pericardial effusion (4.55%) and lymphadenopathy (3.38%). The most common anatomic distribution is bilateral lung (78.2%; 95% CI: 65.69–88.19%). The lesions were mostly located in the periphery (76.95%; 95% CI: 57.43–91.50%) and lower lobes (65.22%; 95% CI: 55.95–73.94%).1
A study from four centers in China analyzed the CT findings in relationship to the time of symptom onset. They demonstrated that CT findings occurred more commonly in those with longer duration following symptom onset. Fifty-six percent of the patients imaged zero to two days after symptom onset had a normal CT compared with only 9% obtained between three and five days after time of onset and 4% between six and 12 days from symptom onset. The CT patterns were similar to those described in the meta-analysis above, with a preponderance of groundglass abnormalities in early disease followed by development of crazy paving and, finally, increasing consolidation later in the disease course.2
CT Findings in GPA
Fewer studies have described the typical CT findings in GPA. Pulmonary nodules and masses are the most common radiologic findings, seen in up to 70% of patients either at presentation or during the course of the disease. Diffuse groundglass opacities and consolidation occur in up to 50% of patients with GPA. The most common distributions of groundglass opacities and consolidations are bilateral perihilar and peribronchovascular. These findings can wax and wane through the course of the disease.
It is important to note that diffuse alveolar hemorrhage (DAH) can mimic these findings, especially because areas of hemorrhage can coalesce and appear as consolidations. A distinguishing feature of DAH would be groundglass opacities with sparing of the subpleural space.3,5
The prevalence of groundglass opacities and consolidations in GPA varies across the literature. Lohrmann et al. described the CT findings of 57 patients with GPA. In 51 patients (89%), the most commonly observed findings were nodules or masses, with a mean of five masses. They were bilateral in 37 patients (70%), and predominantly subpleural and diffuse. They represented isolated findings in 12 patients (23%) and were observed with other findings in 41 patients (77%). Fifteen patients (26%) had areas of groundglass attenuation and were associated with other abnormalities in 11 patients (72%).4