The Case
A 33-year-old Caucasian man with a past medical history of hiatal hernia and peptic ulcer disease was referred to rheumatology for recurrent bouts of acute onset knee pain and swelling. The patient reported he was in his usual state of health until six to seven years earlier when he noticed the insidious onset of worsening arthralgias. Arthralgias began in his knuckles bilaterally and, over the course of several years, affected all the large and small joints of his upper and lower extremities. The pain was described as non-radiating, moderate to severe and aching in nature, with an occasional stabbing sensation. His symptoms were partially controlled with acetaminophen. The patient noted that activity worsened his pain, but alleviated his stiffness. Morning stiffness was reported as lasting two to three hours daily.
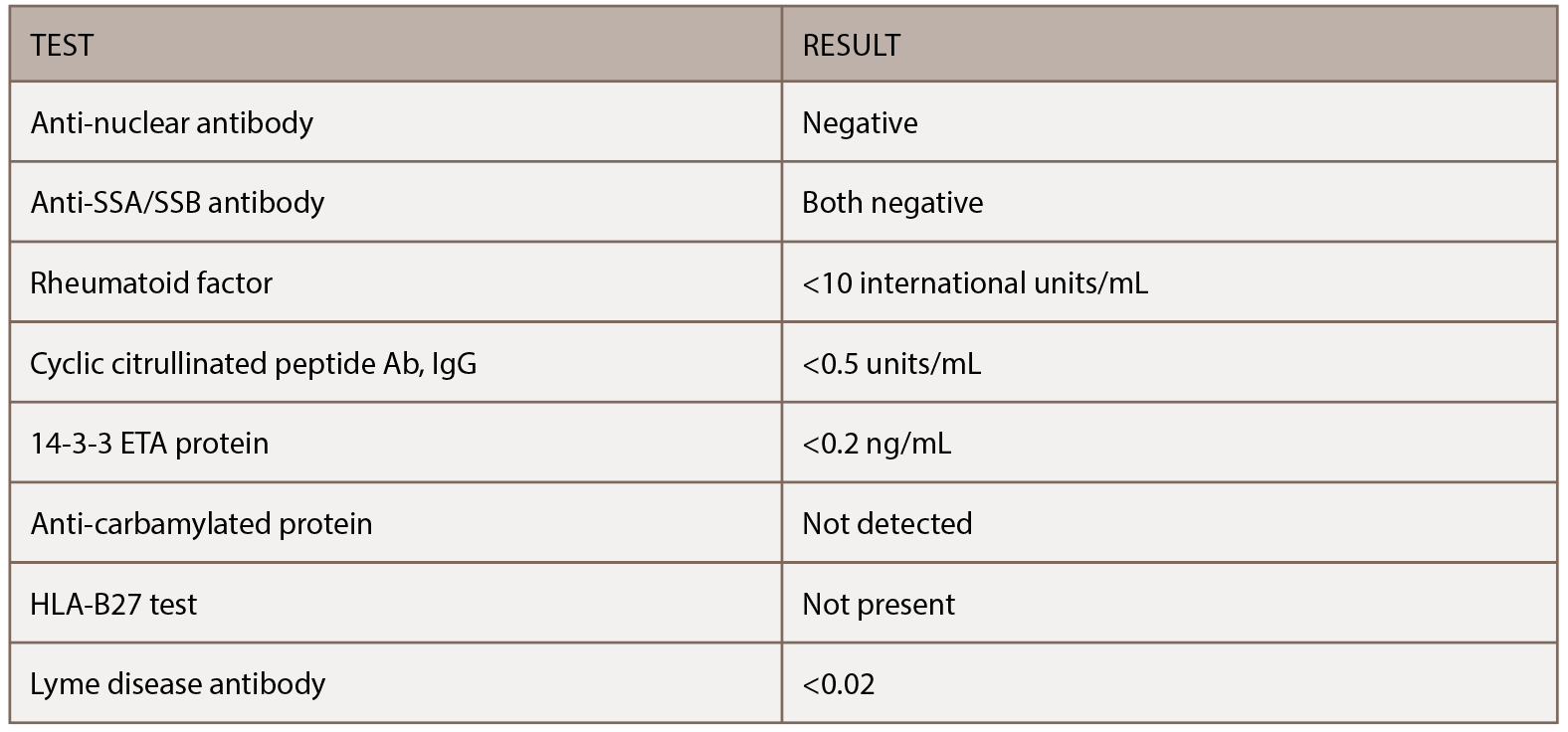
His family history was significant for his father dying at age 57 from hepatitis C-related cirrhosis and his mother dying of an unknown primary cancer at age 42. He previously smoked two packs of cigarettes a day but had quit 14 years earlier. Surgical history was significant for cholecystectomy, which was performed for recurrent bouts of abdominal pain. His initial physical exam demonstrated no evidence of synovitis in his large or small joints beyond tenderness involving the right fourth proximal interphalangeal joint. He had several serologic studies that started the workup noted in Table 1, all of which were negative. X-rays taken of his chest and hands at his initial evaluation proved unremarkable.
One month later, the patient presented for follow-up, two weeks after rapid onset of swelling in both knees. Symptoms started rapidly and ended abruptly two to three days later. The swelling and pain affected his left knee more than the right. Examination of the left knee at this appointment demonstrated some minor swelling and suprapatellar fullness, so arthrocentesis was performed, which yielded no synovial fluid. Given the patient’s report of recurrent bouts of swelling and pain in the left knee, magnetic resonance imaging (MRI) of the left knee was ordered. This report demonstrated mild chondromalacia and a small effusion, but no other significant abnormalities. Additional serologic studies were ordered and were unrevealing.
His symptoms seemed to abate, and at follow-up four months later, he reported having low-grade intermittent flares of arthritis, but the severity had started to improve.
Nine months after his initial evaluation, the patient requested urgent evaluation. He reported the rapid onset of left knee pain and swelling, which was making weight-bearing difficult. He noted that his pain developed in the absence of an antecedent traumatic event or recent infection. He was evaluated within 48 hours and had an almost normal exam, except for slight loss of the peripatellar fossa of the left knee. He showed pictures of his knees on his smartphone taken when the left knee first became acutely inflamed (see Figure 1, left). Based on the photos, his recurrent knee symptoms and the unremarkable rheumatologic workup to date, genetic testing for a periodic fever syndrome was performed. Testing demonstrated heterozygosity for the K695R mutation in pyrin (marenostrin) protein. He was started on colchicine, and although it initially seemed beneficial, his symptoms gradually recurred.